State Use of Behavioral Health Performance Measures in Medicaid Managed Care Contracting
NASHP
APRIL 17, 2023
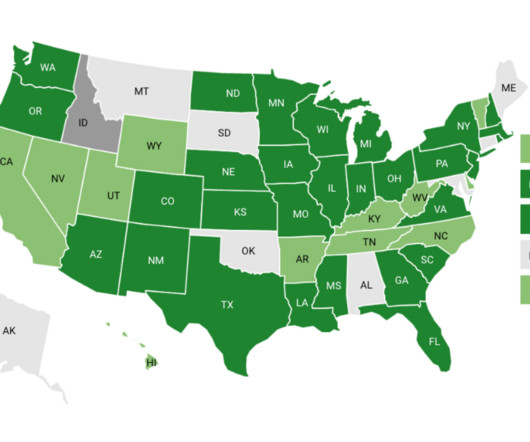
Performance measurement is a pillar of state Medicaid managed care quality improvement and oversight efforts, is often factored into plan payment, and supports public reporting. In states with more than one Medicaid managed care program we reviewed the contracts for all programs.








Let's personalize your content