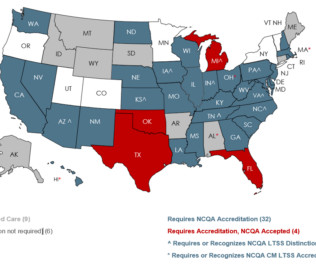
How We Help Medicaid & Long-Term Services and Supports
NCQA
JUNE 27, 2023
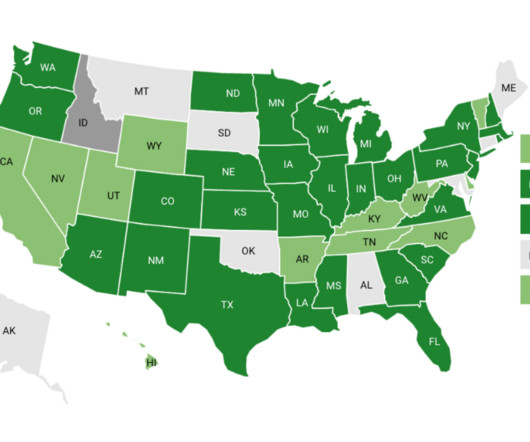
Measuring and Improving Performance: Organizations perform continuous quality improvement of their LTSS program and identify actionable steps to improve care for their members. Accreditation helps accountability and ongoing quality improvement efforts of aging and disability networks.









Let's personalize your content