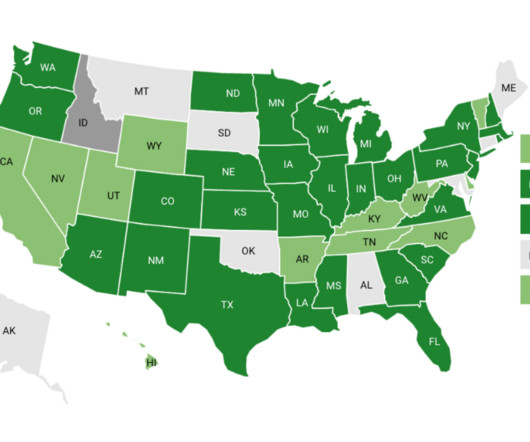
State Use of Behavioral Health Performance Measures in Medicaid Managed Care Contracting
NASHP
APRIL 17, 2023
In states with more than one Medicaid managed care program we reviewed the contracts for all programs. If a measure was collected or used by at least one of the programs, we included it in our data.









Let's personalize your content