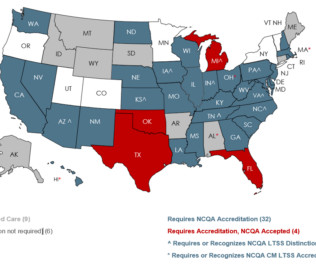
How We Help Medicaid & Long-Term Services and Supports
NCQA
JUNE 27, 2023
More states are contracting with managed care organizations (MCO) to provide Medicaid long-term services and supports (LTSS). How do we know if MCOs are delivering equitable, high-quality care to people receiving LTSS? In July, NCQA will update these programs to further align with best practices and federal regulations.




































Let's personalize your content