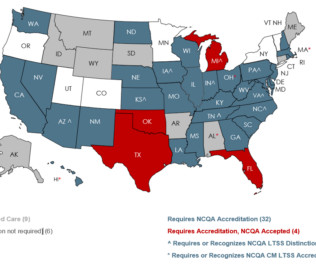
How We Help Medicaid & Long-Term Services and Supports
NCQA
JUNE 27, 2023
In July, NCQA will update these programs to further align with best practices and federal regulations. Here’s how states are harnessing these programs to improve oversight. Service Coordination and Monitoring: “MCOs did not adequately coordinate or monitor beneficiaries’ quality of care.”












































Let's personalize your content