State Approaches to Behavioral Health Measures in Medicaid Managed Care
NASHP
APRIL 17, 2023
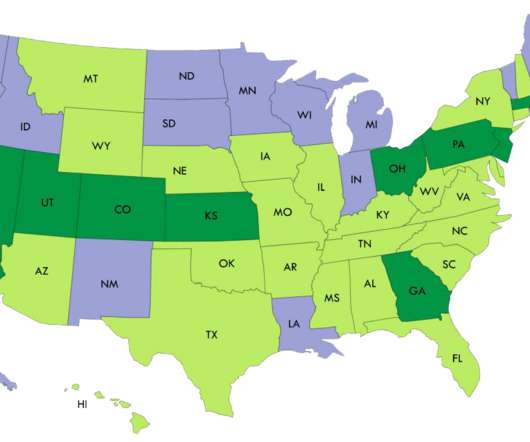
In addition, starting in 2024, federal rules will require states to report performance on some measures, including some behavioral health measures, to the Centers for Medicare & Medicaid Services (CMS). 1] All but one of these Medicaid agencies collected at least one measure of behavioral health performance.
























Let's personalize your content