Managing Managed Care: Closing Gaps in Care for Payers, Providers and Members
GoMoHealth
OCTOBER 20, 2022
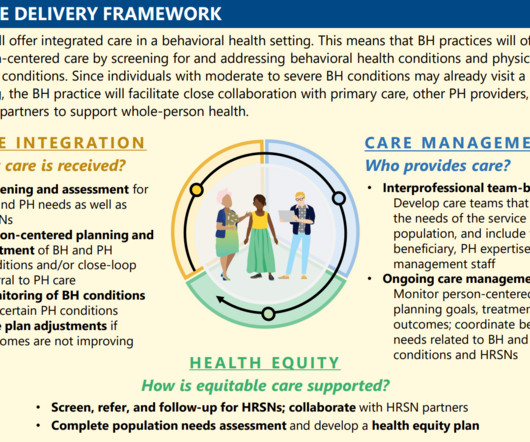
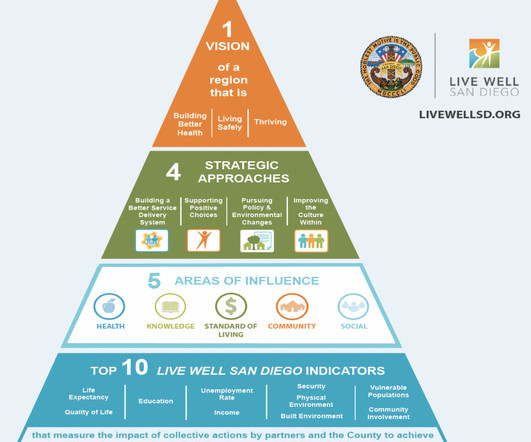
Partnering with Managed Care Organizations and Provider Networks to reduce costs and better manage utilization of health services. By Nakecia Taffa, Quality Improvement and Health Equity Director for GoMo Health. Health Plan Challenges. Failure to Address Healthcare Disparities.














Let's personalize your content