CMMI Prioritizes Multi-Payer Alignment in New Models
NCQA
OCTOBER 31, 2023
And then we’re also developing an approach for certification based on quality improvement and patient experience.”

NCQA
OCTOBER 31, 2023
And then we’re also developing an approach for certification based on quality improvement and patient experience.”
GoMoHealth
OCTOBER 20, 2022
Partnering with Managed Care Organizations and Provider Networks to reduce costs and better manage utilization of health services. By Nakecia Taffa, Quality Improvement and Health Equity Director for GoMo Health. “The Why”. Ability to Foster Trust within Community-Based Organizations and Providers.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.

Sheppard Health Law
OCTOBER 27, 2021
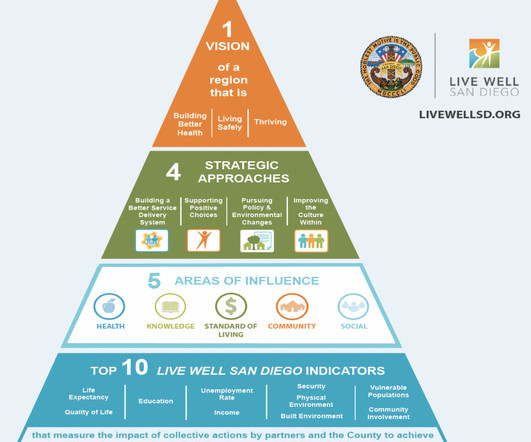
The five strategic objectives for advancing this systemwide transformation include (1) Drive Accountable Care, (2) Advance Health Equity, (3) Support Innovation, (4) Address Affordability, and (5) Partner to Achieve System Transformation. Strategic Objective 3: Support Care Innovations.

NASHP
OCTOBER 20, 2022
As a result, services were better aligned and the MCOs referred CYSHCN to the Title V CYSHCN program for care coordination given the program staff’s expertise in serving this population. Data are central to both direct care coordination service provision, as well as care coordination system monitoring and quality improvement efforts.

NASHP
DECEMBER 10, 2021
ACO Accountable Care Organizations. CBCM Community Based Care Management Program. There are currently some Accountable Care Organizations (ACOs) that cover the cost of CHW services through Medicaid administrative payments. Acronym Guide. APM Alternative Payment Model. CBO Community Based Organization.
NASHP
AUGUST 31, 2023
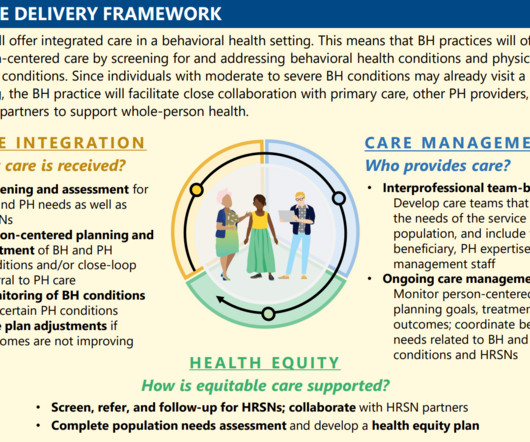
Figure 1 displays a consolidated overview of the “Framework for Public Health-Health Care System Collaboration.” Such models can incentivize health, public health, and social service partners to work collectively to address health-related social needs and work to improve population health outcomes.
HIT Consultant
JANUARY 22, 2024
Implementation (model years 4-8): States will implement a Medicaid payment model that rewards practices for delivering integrated care, while selected practices can also participate in an additional Medicare payment model. Performance-based incentives will further encourage quality improvement throughout the implementation period.
Let's personalize your content