How We Help Medicaid & Long-Term Services and Supports
NCQA
JUNE 27, 2023
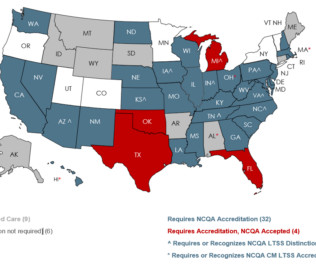
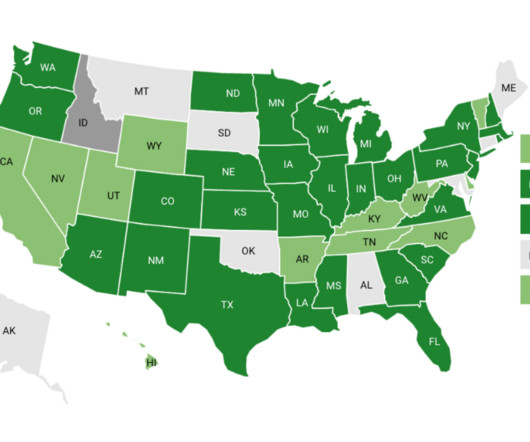
Measuring and Improving Performance: Organizations perform continuous quality improvement of their LTSS program and identify actionable steps to improve care for their members. Hold MCOs Accountable: LTSS Distinction validates that MCOs deliver high-quality, person-centered care to people with complex needs.







Let's personalize your content