CMS Medicaid Proposals Offer Transparency And Accountability, But Compensation Provision Could Cap Business For Cash-Strapped Providers
Home Health Care
APRIL 28, 2023
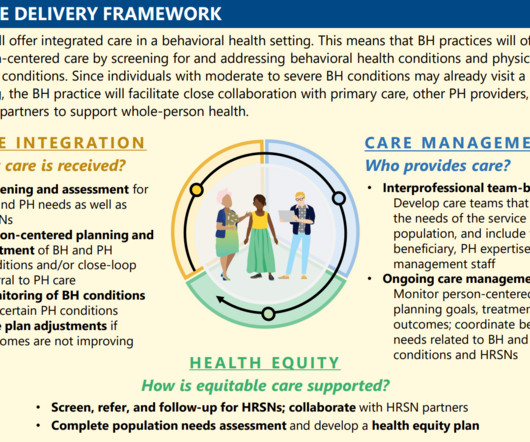
Centers for Medicare & Medicaid Services (CMS) proposed a new rule that would make major changes to the way that home care workers are compensated under Medicaid. The bulk of its business is in Medicaid. Anderson also noted that home care agencies working under Medicaid often vary in size. On Thursday, the U.S.









































Let's personalize your content