What are CY 2024 Policy Updates For MIPS Reporting? (Part I)
p3care
NOVEMBER 10, 2023
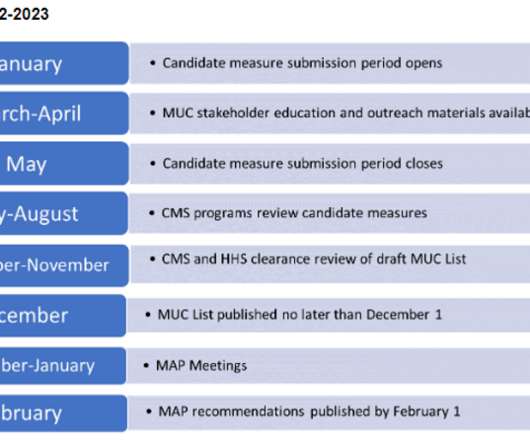
Quality Measure Inventory (for MVPs and Traditional MIPS) We still have 198 quality measures in total, excluding QCDR measures. These measures are customarily approved outside the rulemaking process. Overall, CMS has added 11 quality measures and excluded 11. This new collection type is named ‘Medicare ACO’.











































Let's personalize your content