Centers for Medicare and Medicaid Innovation Center: Equity and Vision
Sheppard Health Law
OCTOBER 27, 2021
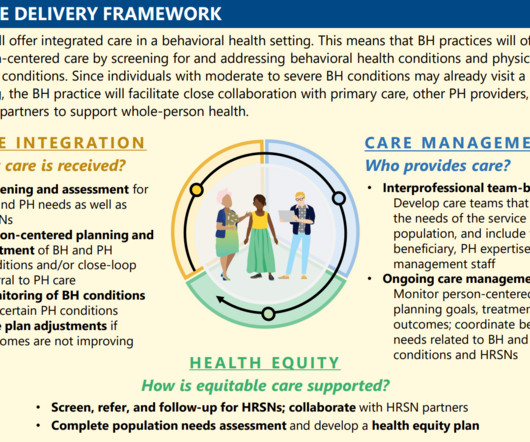
The five strategic objectives for advancing this systemwide transformation include (1) Drive Accountable Care, (2) Advance Health Equity, (3) Support Innovation, (4) Address Affordability, and (5) Partner to Achieve System Transformation. Strategic Objective 1: Drive Accountable Care.










Let's personalize your content