CMS Unveils “Innovation in Behavioral Health” Model to Tackle Dual Mental and Physical Health Challenges
HIT Consultant
JANUARY 22, 2024
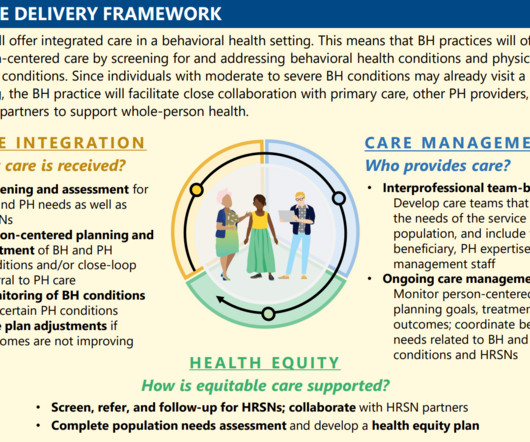
What You Should Know: – The Centers for Medicare & Medicaid Services (CMS) has taken a bold step towards improving care for individuals with both mental health conditions and substance use disorders (SUD), announcing the “ Innovation in Behavioral Health (IBH)” Model.














Let's personalize your content