CMS Medicaid Proposals Offer Transparency And Accountability, But Compensation Provision Could Cap Business For Cash-Strapped Providers
Home Health Care
APRIL 28, 2023
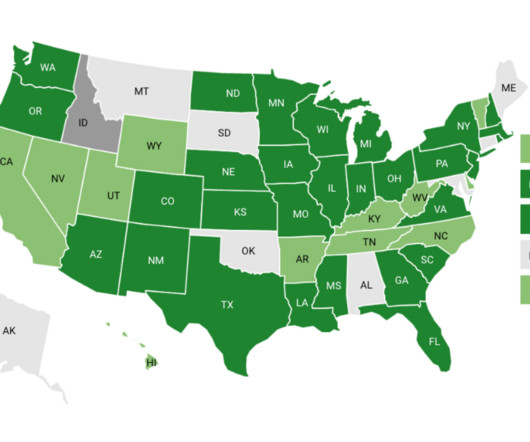
It’s a step towards additional transparency and accountability, including state, payer and provider,” he told HHCN. “I Aside from the 80% provision, the proposal also establishes a new strategy for oversight, monitoring, quality assurance and quality improvement for HCBS programs. and North Carolina.










Let's personalize your content