State Use of Behavioral Health Performance Measures in Medicaid Managed Care Contracting
NASHP
APRIL 17, 2023
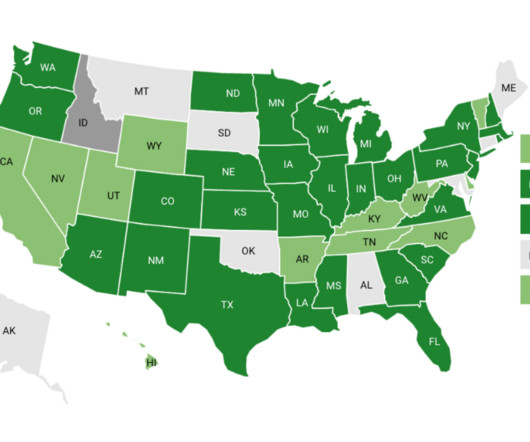
Performance measurement is a pillar of state Medicaid managed care quality improvement and oversight efforts, is often factored into plan payment, and supports public reporting. 42 Medicaid agencies collected at least one measure of behavioral health performance. Check out the map and chart below for an overview of our findings.







Let's personalize your content