CMMI Prioritizes Multi-Payer Alignment in New Models
NCQA
OCTOBER 31, 2023
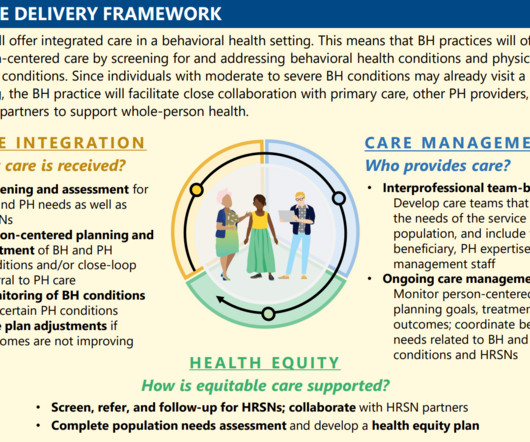
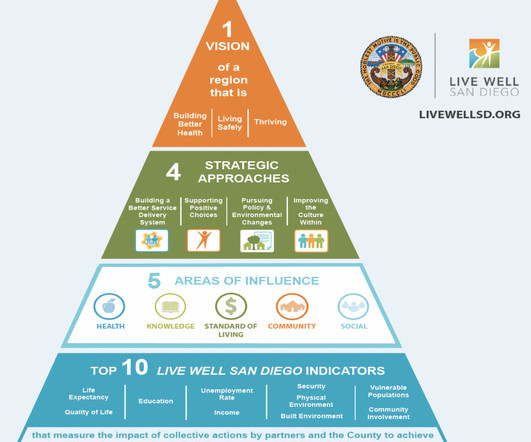
The Innovation Center also released the Making Care Primary (MCP) model and the GUIDE model this year, innovative solutions to achieve multi-payer alignment and focus on populations that have historically been underfunded in health care.























Let's personalize your content