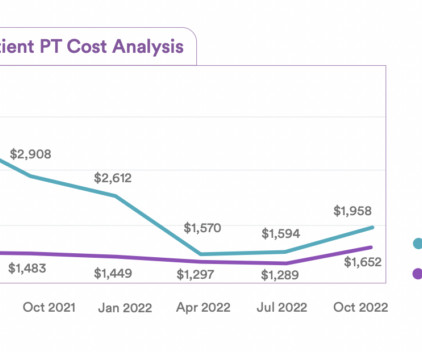
Study: In-Home Outpatient PT Reduces Costs By 52% Compared To Traditional Home Health Services
Home Health Care
JUNE 1, 2023
The study — done in conjunction with the nonprofit hospital system Hoag Hospital — was conducted between 2021 and 2023. According to data from Hoag Orthopedic Institute (HOI), traditional home health PT for post-surgical rehabilitation in 2021 accounted for 10.4% of the total episode cost for the health network.












Let's personalize your content