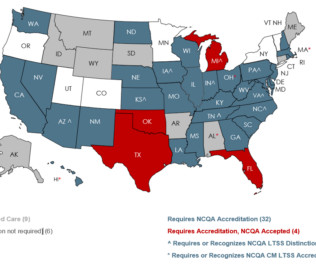
How We Help Medicaid & Long-Term Services and Supports
NCQA
JUNE 27, 2023
Service Coordination and Monitoring: “MCOs did not adequately coordinate or monitor beneficiaries’ quality of care.” Measuring and Improving Performance: Organizations perform continuous quality improvement of their LTSS program and identify actionable steps to improve care for their members.

















Let's personalize your content