Mary Madison, RN, RAC-CT, CDP
Clinical Consultant – Briggs Healthcare

“The COVID-19 pandemic had a big impact on assisted living (AL), a vital setting in long-term care (LTC). Understanding the strengths and opportunities for improvement through practice, policy, and research are essential for AL to be prepared for the next pandemic and other challenges. AL communities experienced the pandemic in unique ways, because of varying regulatory environments, differences in familiarity with using and procuring personal protective equipment not typically used in AL (such as N95 masks), loss of family involvement, the homelike environment, and lower levels of licensed clinical staff. Being state rather than federally regulated, much less national data are available about the COVID-19 experience in AL. This article reviews what is known about cases and deaths, infection control, and the impact on residents and staff. For each, we suggest actions that could be taken and link them to the Assisted Living Workgroup Report (ALW) recommendations. Using the Center for Excellence in Assisted Living (CEAL) 15-year ALW report, we also review which of these recommendations have and have not been implemented by states in the preceding decade and half, and how their presence or absence may have affected AL pandemic preparedness. Finally, we provide suggestions for policy, practice, and research moving forward, including improving state-level reporting, staff vaccine requirements, staff training and work-life, levels of research-provider partnerships, dissemination of research, and uptake of a holistic model of care for AL.”
This special article was published in the December 30, 2022 edition of JAMDA (Journal of Post-Acute and Long-Term Care Medicine). The 5-page PDF article can be found here.
“SARS-CoV-2 (COVID-19) is attributed to more than 1,000,000 US deaths, of which 75% were among persons aged 65 years and older. Estimates are that assisted living (AL) saw nearly 30,000 resident COVID-19 deaths between January 2020 and March 2021. AL is a vital part of long-term care (LTC) in the United States and serves 918,700 residents in 31,400 AL communities. AL began decades ago with the idea of person-centered care and with a population much healthier than today’s AL residents.4 The medical complexity, frailty, cognitive, and functional status of this population places them at high COVID-19 risk.
Understanding the full impact of the pandemic on AL is important but challenging. AL is regulated by state laws and must follow state infection control prevention guidelines, which vary in terms of data reporting, protective restrictions, oversight, and assistance. Nevertheless, it is essential that the AL COVID-19 experience be understood to prepare for future emergencies.”
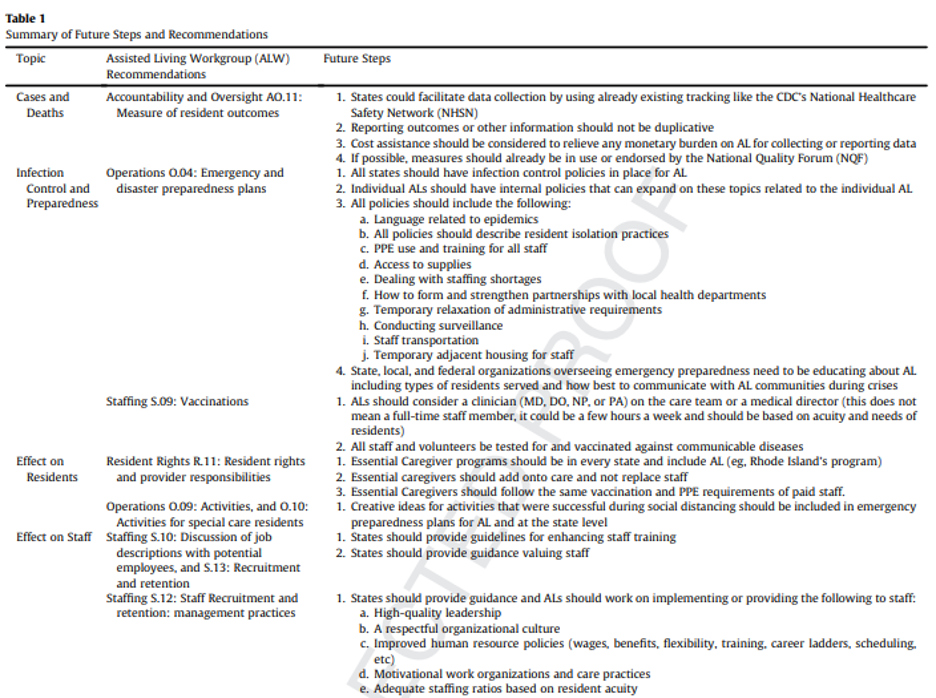
I strongly encourage you to review and share the article with your colleagues. There is a lot of important information in the article, including a table of the AL Workgroup Recommendations and Future Steps (found on page 3 of the PDF).
“Lastly, the pandemic has shown that AL is a vital part of long-term care and the entire health care continuum. CEAL advocates strongly for the holistic, PCC (person-centered care) model of care that is the hallmark of AL. Research is needed to document the importance of this model of care, including the preservation of resident and staff well-being in the face of a deadly disease that targeted this demographic. Policy is needed to support care that melds social and medical needs, both because it creates the highest quality of care and quality of life for residents and because it best prepares these communities to face crises, lowering risks of infection for everyone.”
