State Medicaid agencies are taking proactive steps to ensure quality of care and access to behavioral health services. They are accomplishing this by considering plan performance in the provision of behavioral health services as a determinant of payment for the plans. It is expected that these states will continue to refine their models, and other states may follow suit. To support these efforts, NASHP analyzed information about current state approaches to tying payment to performance in delivering behavioral health services. Below is an overview of the policy choices states have made. (Access the complete set of information NASHP collected and related analyses.)
Most States Offer Managed Care Plans Payment Incentives to Improve Behavioral Health Services
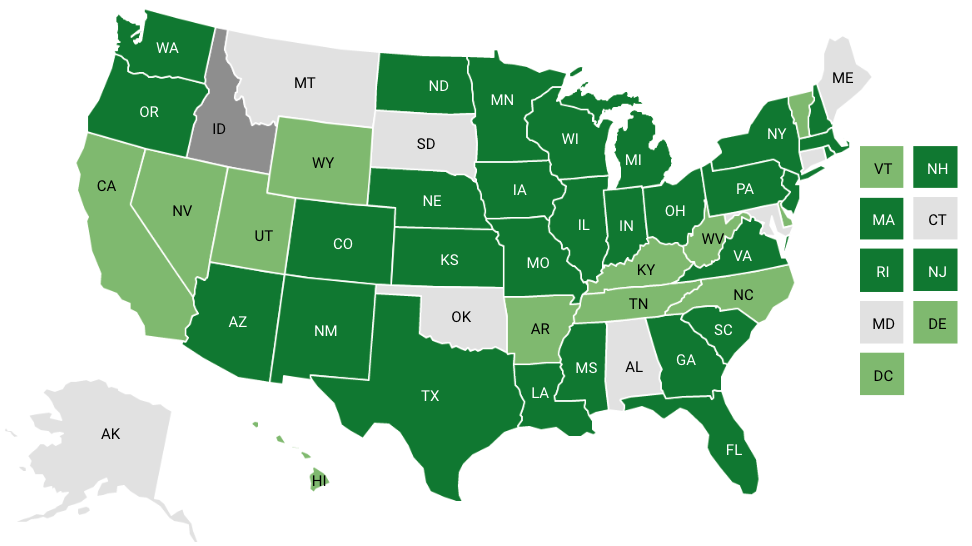
In our review of Medicaid managed care contracts, we identified 29 states that factored plan performance on at least one behavioral health measure into their payments to managed care organizations (MCOs) that deliver a comprehensive package of benefits. Four of these 29 states have also integrated this approach into their contracts with prepaid inpatient health plans (PIHPs) that solely deliver behavioral health services. A few states also implemented innovative strategies, such as using payment incentives to improve health equity or factoring plan performance into other aspects of plan payment (for example, medical loss-ratio calculations).
States established a wide range of incentives, with considerable variation among them. Some states attached incentives to individual measures, while others grouped measures and rewarded performance in a category. Many funded the incentives by withholding a percentage of the amount paid to contracted plans, and some of these distribute unearned withheld funds to the highest performing plans.
As you can see, states have adopted a diverse range of strategies. Below are some examples of how states have linked plan payment to performance in delivering behavioral health services.
State Use of Behavioral Health Performance Measures in Medicaid Managed Care Contracting
New Hampshire Rewards Performance on Groups of Measures and Redistributes Unearned Funds
According to its state fiscal year 2021 Withhold and Incentive Guidance, New Hampshire withheld 2 percent of capitation rates. MCOs may earn the withheld amount by performance on six measures that have been divided into three categories: quality improvement (three measures), care management (one measure), and behavioral health (two measures). The behavioral health measures were:
- Follow-up after emergency department visit for alcohol and other drug abuse or dependence — seven days
- Metabolic monitoring for children on antipsychotics
The Medicaid agency establishes the percentage of the withheld amount that may be earned through performance in each category. In 2022, behavioral health performance was worth 25 percent of the withheld amount. The agency also establishes minimum performance standards and performance goals for each measure. To earn any of the amount assigned to a category, an MCO must meet the minimum performance standards of all measures in the category. The exact amount of withheld funds an MCO may earn in each category depends on how closely that MCO’s performance comes to meeting (or exceeding) the annual goals for the measures in the category.
After New Hampshire determines how much of the withheld funds MCOs earn in a category, the Medicaid agency uses any unearned funds to create an incentive pool for that category. If a pool is created, the highest performing MCOs may earn an incentive bonus from that pool. To qualify for the bonus, an MCO must meet the minimum performance standards for all measures in all three categories. They must also meet the annual goals for all measures in the incentive pool category (for example, the two measures in the behavioral health category). The size of the incentive payment is determined by an MCO’s performance, the amount of funding in the pool, and the number of MCOs that qualify for a performance bonus.
Minnesota Factors MCO Performance in Addressing Health Equity, Including Behavioral Health Equity, into Its Payment Policies
Minnesota’s incentive payment model, like many others, is funded by a capitation withhold that MCOs serving children and families may earn through their performance on 10 measures, including two behavioral health measures:
- Follow-up after hospitalization for mental illness (seven and 30 days)
- Initiation and engagement of alcohol, opioids, and other drug dependence treatment
According to Minnesota’s 2022 Technical Specifications, an MCO’s performance on six of the measures, including the behavioral health measures, is assessed on both achievement and improvement in the MCO’s performance in delivering services to five groups of enrollees formed based on race and ethnicity. These groups are listed here, the first group is referred to as the reference group, the remaining four are referred to as comparison groups.
- Non-Hispanic white race
- Black/African American race
- Native American/Alaskan Native race
- Asian/Pacific Islander race
- Hispanic ethnicity (all races)
If an MCO’s overall contract year performance on a measure does not decline compared to base-year performance (2019 was the baseline for the 2022 contract year), then the MCO can earn points for having moved its performance for the four comparison groups closer to its performance for the reference group. The agency established this gateway requirement to ensure that MCO efforts remain focused on service delivery quality for all. The requirement also protects against an MCO earning points by lowering its reference rate rather than increasing its comparison group rates.
If the gateway requirement is met, then the agency awards points using one of three methods, depending on scenarios defined by the diversity and size of the five MCO populations. The total number of points earned governs the percent of its withheld funds an MCO receives. The three methods are:
- An MCO’s baseline performance for the reference group is better than its baseline performance for the comparison group. (In this case, the disparity gap is the difference between the two rates. An MCO earns points if the disparity gap in the contract year is smaller than it was in the baseline year. The MCO loses points if the gap is larger.
- An MCO’s baseline performance for a comparison group is equal to or better than its performance for the reference group. In this case, an MCO earns points for performance in delivering services to that comparison group if its overall performance for all enrollees (including those whose race is not recorded in the data) is better in the contract year than it was in the baseline year.
- There are fewer than 30 MCO members in the comparison group who meet the criteria for inclusion in the measure’s denominator. In this case, an MCO earns points by increasing the number of members in the numerator (for example, increases the number of comparison group members engaged in treatment from four in the baseline year to six in the contract year).
Colorado Factors MCO Performance, Including Performance in Delivering Behavioral Health Services, Into Its Medical Loss Ratio Calculations
Federal rules require states to require MCOs to calculate the percentage of capitation payments they spend on clinical services and quality improvement each year (the percentage is referred to as the medical loss ratio or MLR). States are allowed to set an MLR standard of 85 percent or more. Colorado Medicaid leverages its MLR policies to create an incentive for plans to improve performance. The state has established 89 percent as the MLR requirement for the two MCOs that participate in their program. MCOs can earn a lower percentage (down to 85 percent) by achieving agency-established performance goals on a set of measures. The effect of the reduction is to increase the amount of income that an MCO may retain. The measures differ between the two plans. One is assessed on its performance on three measures, including one behavioral health measure. The other MCO is assessed on its performance on four measures, including one behavioral health measure. Colorado used “initiation and engagement of alcohol and other drug dependence treatment” as the behavioral health measure for both plans.
States Continue to Evolve Their Payment Models
Most states have incorporated behavioral health performance into their efforts to use payment to create incentives for Medicaid managed care plans to improve performance. While most have chosen to use incentives to reward improvements in access and quality, others have chosen to pursue other policy goals or extend the model into new policy areas, such as increasing health equity or the use of value-based payment for providers.
Acknowledgements
The National Academy for State Health Policy (NASHP) would like to thank the state officials from Colorado, Minnesota, and New Hampshire who reviewed a draft of the document. In addition, we thank Health Resources and Services Administration Project Officer Kelli Crosby and her colleagues for their feedback and guidance. Finally, the author wishes to thank Hemi Tewarson, Sandra Wilkniss, and Laura Galbreath of NASHP for their contributions to the paper, as well as Sam Mermin for his assistance with the 50-state scan. This project was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under co-operative agreement number UD3OA22891, National Organizations of State and Local Officials. The information, content, and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS, or the U.S. government.