This is one section of Modernizing Behavioral Health Systems: A Resource for States. See the full resource guide.
As major purchasers, administrators, and regulators of behavioral health treatment and supports, states play a critical role in system transformation. State leaders can use these levers to develop a modern behavioral health system with equitable access to high-quality services and supports, including establishing a statewide vision, driving reform through payment and delivery transformation (including public and commercial payer approaches), investing in infrastructure (including data and workforce) and provider capacity, reducing administrative burden while retaining quality oversight, and effectively communicating with key partners to inform and implement that vision. These examples illustrate how states have taken a comprehensive approach through overall system transformation and/or strategic disruptive investments.
Examples of Comprehensive State Approaches
Massachusetts
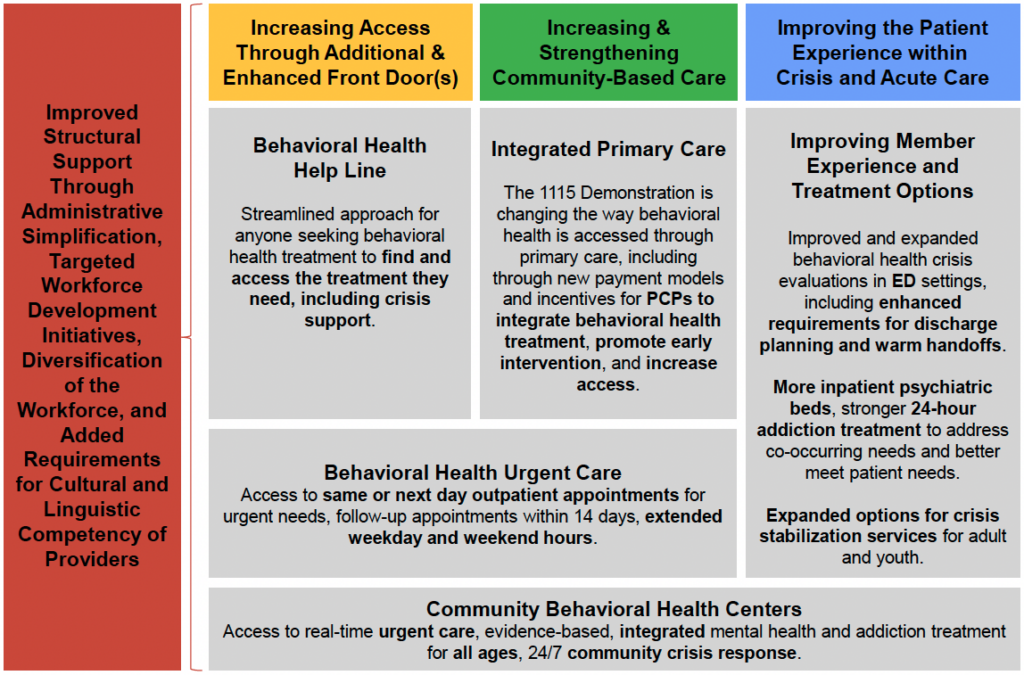
Massachusetts began implementation of the Roadmap for Behavioral Health Reform in 2023, a multi-year blueprint championed by the governor and led by the secretary of health and human services that was informed by input from almost 700 individuals, families, providers, and other interested partners. Along with the Mental Health ABC Act: Addressing Barriers to Care for Mental Health, enacted in August 2022, the roadmap sets the vision and invests in a “no wrong door” approach to improved access to quality behavioral health care in the state. Details on structural reforms and service improvements are found in the box below.
Reforms through the Behavioral Health Roadmap
North Dakota
North Dakota’s Governor Doug Burgum included behavioral health in his five strategic initiatives for the state. Based on a comprehensive state study of services, utilization, and expenses, the state built a comprehensive plan and is tracking through a project dashboard quarterly progress on benchmarks and indicators of 13 aims. The governor-appointed Behavioral Health Planning Council is responsible for overseeing the strategic planning process, providing guidance on the prioritization and direction of objectives, and monitoring progress towards the established strategic goals.
Aims of North Dakota's Plan for Behavioral Health
- Develop and implement a comprehensive strategic plan.
- Invest in prevention and early intervention.
- Ensure all North Dakotans have timely access to behavioral health services.
- Expand outpatient and community-based service array.
- Enhance and streamline system of care for children with complex needs and their families.
- Continue to implement and refine the current criminal justice strategy.
- Engage in targeted efforts to recruit and retain a qualified and competent behavioral health workforce.
- Continue to expand the use of telebehavioral health interventions.
- Ensure the system reflects its values of person-centeredness, health equity, and trauma-informed approaches.
- Encourage and support communities to share responsibility with the state for promoting high-quality behavioral health services.
- Partner with tribal nations to increase health equity for American Indian populations.
- Diversify and enhance funding for behavioral health.
- Conduct ongoing, system-wide, data-driven monitoring of need and access.
Source: North Dakota Behavioral Health Plan Project Dashboard
North Carolina and New York
North Carolina and New York included extensive multi-year investments in their fiscal year (FY) 2024 budgets aimed at building the behavioral health continuum. In addition to expanding Medicaid, North Carolina’s FY2024 budget allocates over $835 million for mental health and substance abuse investments under Medicaid. This funding encompasses several initiatives, such as raising rates for behavioral health services to match or surpass the Medicare fee schedule by 120%, offering bonuses and incentive pay for service providers, providing support services for families and children with mental health needs, establishing community-based care for individuals with intellectual and developmental disabilities, and facilitating the construction of a regional children’s behavioral health hospital.
New York
New York’s FY 2024 budget includes $1 billion investment in operating funding to establish 3,500 residential units; increase inpatient capacity; and significantly expand outpatient services. The plan also includes investments in peer-based outreach, an expansion of school-based mental health services, and provisions to close gaps in insurance coverage for behavioral health services. The budget provides greater authority to the State Mental Health Office to sanction community hospitals that do not have the number of psychiatric beds cited in their operating certifications and to expand the office’s loan repayment program for licensed mental health professionals.
Michigan
Similarly, Michigan’s FY2023 and FY2024 budgets include close to $600 million to build behavioral health capacity — especially in the community. Nearly $278 million of the $364 million in the FY2024 budget is targeted to expanding certified community behavioral health centers; $72 million is for mental health care and facilities in educational settings, $20 million for telemedicine infrastructure, and $10 million to implement employee wellness supports to address stress and burnout. These investments build on a supplemental spending bill providing $238.1 million for mental health infrastructure enacted in 2023 for pediatric behavioral health center, crisis stabilization units, and residential treatment facilities, which are a step down from inpatient care.
Texas
Texas lawmakers in the 88th legislative session made a historic investment of $11.68 billion for behavioral health, an increase of more than 30% from the previous session.Investments are targeted at state hospital and mental health facilities, children’s mental health and school safety, and building out access to intensive services in community (such as crisis support services).
Colorado
Colorado is engaged in multi-pronged behavioral health reform. This includes alignment across the state Medicaid and behavioral health administrations, including shared systems and shared accountability, and a unified contracting approach across all relevant state agencies to create a unified network.
In addition, the 2022 Bill 22-181 allocated $36 million in one-time federal stimulus funds to reinforce the behavioral health workforce that serves people of all ages, including pregnant and parenting people, infants, children, and older adults. The Behavioral Health Administration (BHA) developed a workforce plan that aims to strengthen the career pipeline and publicly fund behavioral health providers, remove barriers for those entering the field, and reduce the administrative burdens that impede entry and retention of workers. Colorado also includes traditional workforce and labor agencies in its partnerships to build the behavioral health workforce. Aligning work with the Colorado Workforce Development Council and the Colorado Department of Labor and Employment allows for coordinated development of career pathways and apprenticeships in behavioral health care. Additionally, the BHA will coordinate outreach and marketing efforts to promote all professions in the behavioral health field.
Examples of Cross-Cutting Approaches and Tools
Improving Quality via Medicaid Managed Care Contracting
States are expanding use of behavioral health performance measures in managed care contracting and linking Medicaid managed care plan payments to performance in behavioral health service delivery. Here are a few examples:
- New Hampshire rewards performance on certain measures (including seven-day follow-up after emergency department visit for alcohol and other drug abuse or dependence and metabolic monitoring for children on antipsychotics) and redistributes unearned funds through its capitated payment rates.
- Minnesota includes managed care performance in its equity approach through an incentive payment model, and two of the state’s 10 performance measures for managed care organizations (MCOs) serving children and families are specific to behavioral health (including follow-up after hospitalization for mental illness (seven and 30 days) and initiation and engagement of alcohol, opioids, and other dru Specifically, an MCO’s performance on six of the 10 measures (including the behavioral health measures) is assessed on both achievement and improvement in performance in delivering services to four groups of traditionally underserved enrollees formed based on race and ethnicity (compared to a non-Hispanic White reference group).
- In Colorado, Medicaid leverages its medical loss ratio (MLR) policies to incentivize MCOs’ performance. Participating MCOs can earn a lower percentage (85%, down from the state’s established 89% MLR requirements) by improving performance on key measures, thereby increasing the amount of income the MCO may retain. For the two participating plans, measures differ, but both include one behavioral health measure.
Moving toward Parity
Nearly half of states have adopted model legislation to address coverage parity. Two states have pursued more innovative approaches and were highlighted in a NASHP report on increasing access to behavioral health care.
- Washington enacted legislation in 2022 that aligns coverage of the full range of behavioral health emergency and urgent care services with coverage of the full range of medical emergency and urgent care services and protects consumers of behavioral health crisis services from out-of-network charges, thereby aligning state law with the federal No Surprises Act and Mental Health Parity and Addiction Equity Act. This law advances consumer protections and access to behavioral health crisis services in facilities and appears to apply across payers; however, clear federal guidance on the latter would benefit all states.
- As part of the sweeping mental health legislation enacted in Massachusetts, the state has bolstered parity implementation and enforcement tools, including quicker resolution of parity complaints, greater reporting and oversight of carrier’s policies and processes, and establishment of reasonable penalties and other remedies to address noncompliance. In addition, through its new 1115 demonstration extension and “Roadmap for Behavioral Health Reform,” the state is phasing in a new integrated primary care payment and reimbursement structure. The state is investing $115 million per year in primary care through a new value-based sub-capitation model that requires providers to meet certain standards for access and team-based integrated care while providing more flexibility. Commercial insurance carriers will be strongly encouraged to align with these payment policies.
Workforce and Provider Capacity-Building
The most significant rate limiter to modernizing the behavioral health system is establishing needed workforce to deliver high-quality care where and when people need it. As states work to address this chronic and increasingly challenging problem, they can pursue multiple-reinforcing strategies. These can include administrative simplification, funding, and financing approaches to enhance provider capacity to engage in services, expand the workforce of individuals with lived experience, and optimize traditional workforce development levers such as loan repayment/forgiveness, scholarships, pipeline approaches, and addressing scope of practice barriers. Examples include:
- The Ohio Department of Mental Health and Addiction Services partnered with other state agencies, including Job and Family Services, Medicaid, Youth Services, Developmental Disabilities, Health, and Ohio Family and Children First, to develop a Child and Adolescent Behavioral Health Center of Excellence (COE) dedicated to training and supporting the children’s behavioral health workforce in Ohio. The COE works to assist the state in system transformation efforts by providing technical assistance, training, professional development, coaching, consultation, evaluation, fidelity monitoring, and continuous quality improvement to build and sustain capacity in delivering evidence-based practices to fidelity within a system of care framework.
- Georgia has a long history of including peer support in its behavioral health system. In addition to providing training and certification for peer support specialists, Georgia fosters a variety of professionalization supports, such as training in advocacy, leadership, and grassroots initiatives. Peer support spans all aspects of Georgia’s crisis system, including call center staff, certified peer specialists in every mobile crisis team, behavioral health crisis centers, and crisis stabilization units with living room models (an alternative space to the emergency department that is intentionally designed to be inviting and staffed with clinicians and peers, fostering a sense of safety and support). Warmlines provide Georgians the opportunity to receive peer support over the phone 24 hours a day.
- The Michigan State Loan Repayment Program is structured to recruit and retain high-demand clinical social workers and mental health counselors. In Michigan, a mental health provider could receive one of the highest loan assistance amounts in the country — up to $300,000 over 10 years. The provider could participate in the loan repayment program for a decade, which is enough time to settle in a new community. The state also incorporated workforce strategies within its overhaul of the pediatric behavioral health system, proposing initiatives such as expanding the funding of paid internships and providing training for new providers in youth behavioral health shortage areas.
Additional Resources
- The Mental Health Resource Guide for State Policymakers addresses challenges and solutions in mental health policy, encompassing social isolation, maternal mental health, social determinants of mental health, and mental health insurance parity. It is the result of a nine-month partnership between the Council of State Governments and The Commonwealth Fund.
- The Behavioral Health Strategy outlines CMS’ focused efforts to target substance use disorders, pain treatment, and mental health care while aligning with CMS’s broader focus on coverage, quality, equity, and data analytics.
- Medicaid Forward: Behavioral Health is a framework developed by the National Association of Medicaid Directors, offering a spectrum of strategies for states to improve the health and accessibility of behavioral health services for Medicaid beneficiaries. These strategies encompass preventive measures, health promotion initiatives, and tailored treatments for specific subpopulations within the Medicaid program.
Acknowledgement
NASHP expresses its gratitude to the Commonwealth Fund for generously supporting this resource and to the Behavioral Health Modernization Learning Collaborative for their active involvement.
Special appreciation goes to state leaders and experts including Suzanne Fields and Rebecca Boss who contributed valuable input and feedback to this resource. The strategies and examples within were identified through rigorous research, informational interviews with leaders in state public health, mental health, substance use, Medicaid, and related agencies. This collaborative effort involved a state leader workgroup, expert-informed multi-state convenings, and focused technical assistance with five states. NASHP also thanks Josh Rohrer for his contribution to this resource while on staff at NASHP.

