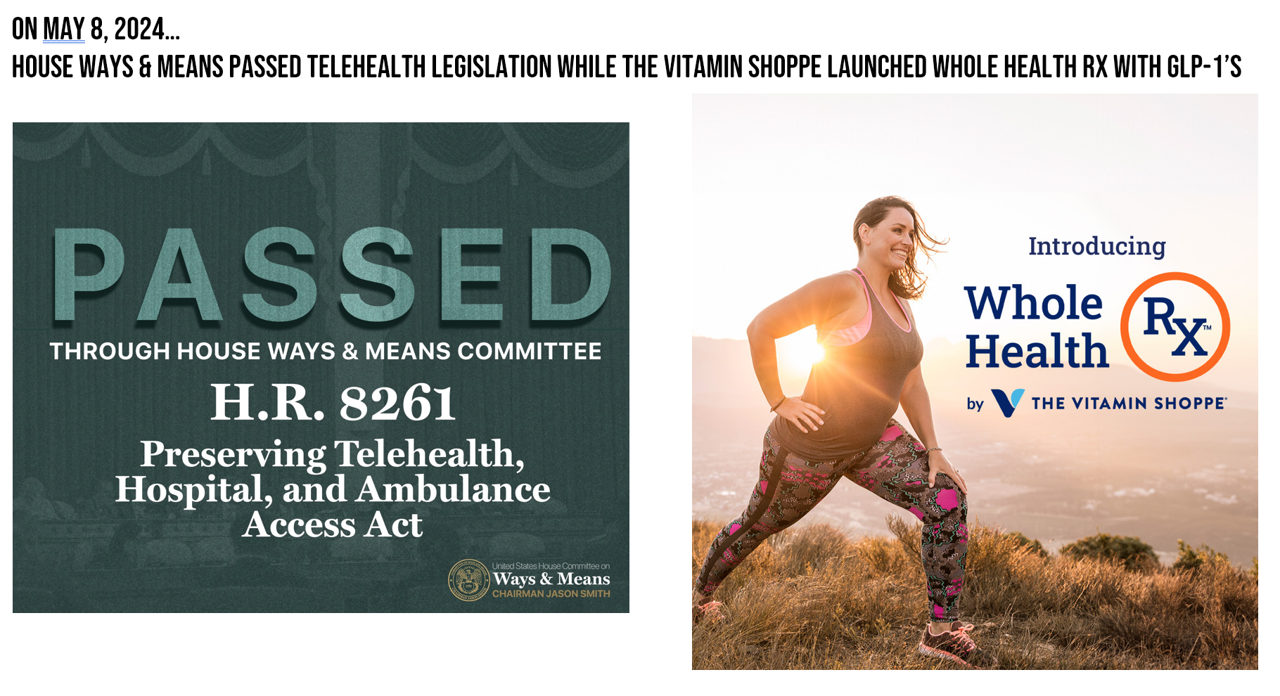
Yesterday, the U.S. House Committee on Ways and Means passed six pieces of legislation that would bolster telehealth in the U.S. for the next two years, assuring several aspects of access for health citizens across the country.
“One of our top priorities on this Committee is helping every American access health care in the community where they live, work, and raise a family,” Committee Chairman Jason Smith (R-Mo.) explained in his introductory statement. Being from Missouri, Chairman Smith is especially keen on the role virtual care and telehealth can play to expand access to the under-served in the U.S. “In rural America and small towns, families often struggle to get health care…The lack of access to emergency and outpatient services and preventative care is one of the reasons why rural Americans have a 43 percent higher mortality rate than urban Americans. Congress has a responsibility to the millions of patients living in rural America to make sure they have access to reliable, quality, lifesaving care.”
Here is a video of Chairman Smith’s initial remarks recorded prior to the six legislative mark-ups expanding on these observations and objectives.
The six pieces of telehealth policy cover:
- The Preserving Telehealth. Hospital, and Ambulance Access Act (HR 8261) – addressing Medicare telehealth for Hospital-at-Home flexibilities for five years, as well as payments for rural hospitals and ambulance services
- The Preserving Emergency Access in Key Sites (PEAKS) Act (HR 7931) – permanently expanding Medicare emergency ambulance coverage for mountainous communities
- The Rural Hospital Stabilization Act (HR 8245) – providing grants to aid rural hospitals stabilize finances and continuing to serve patients
- The Ensuring Seniors’ Access to Quality Care Act (HR 8244) – offering more training opportunities for Americans working to become Critical Nursing Aides (CNAs)
- The Rural Physician Workforce Preservation Act (HR 8235) – to allow more med students to complete graduate medical education in rural hospitals (for residency)
- The Second Chances for Rural Hospitals Act (HR 8246) – to bring back critical emergency and outpatient care to rural communities whose local hospitals had closed down, converting to a new federal Rural Emergency Hospital (REH) designation.
Taken together, these six policies save some key pandemic-era waivers such as eliminating geographic requirements and expanding origination sites for telehealth services. Some of the policies would add to the supply of licensed health care workers to provide telehealth services, and to bolster rural clinics and Federally Qualified Health Centers to offer (and be covered for) virtual care under Medicare.
As I explained in this post on Health Populi about one month ago, A vote for telehealth is a vote for patients’ and clinicians’ well-being.
Health Populi’s Hot Points: While we are on pins and needles awaiting Congress’s continued attention to getting telehealth legislation passed, the health care landscape continues its inevitable march to where the money and market opportunities lie — and in 2024, we observe the mash-up of GLP-1 antagonists with telehealth services.

Yesterday, along with the House’s legislative moves toward virtual care assurance, we received news that The Vitamin Shoppe, a retail health provider, launched what it terms a “holistic telehealth service” featuring GLP-1 meds such as Ozempic, Mounjaro, and lower-cost options in the portfolio of new weight-loss drugs.
Termed Whole Health Rx(TM), this program will bring together the prescription drugs (prescribed through licensed medical providers) combined with The Vitamin Shoppe’s nutrition education resources, nutrition supplements, and weight management support across the omnichannel — with an emphasis on a virtual care platform connecting consumer-patients with licensed healthcare providers.
The Vitamin Shoppe’s weight loss program coupled with GLP-1s joins over a dozen already operating in the U.S., platforming telehealth with weight loss and the fast-growing medicine category — such as Eli Lilly Direct, the pharmaceutical company planning to go direct-to-consumer to channel patients’ access to and use of Zepbound for weight loss (partnering with Amazon’s pharmacy for delivery).
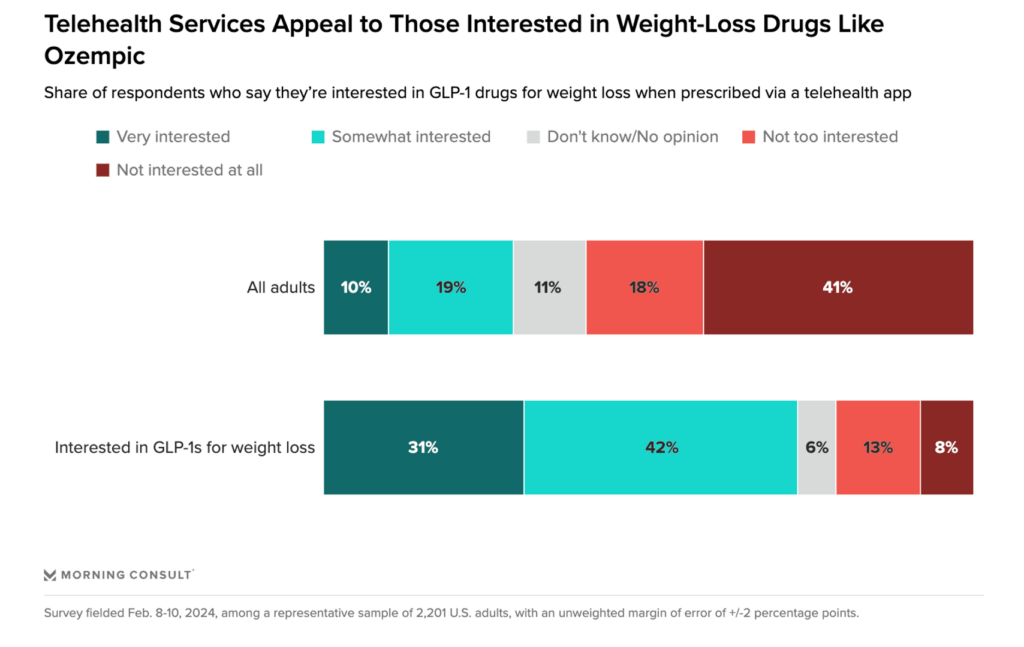
A Morning Consult poll conducted in February 2024 found that consumers would be keen to engage with the new GLP-1 medicines for weight loss when coupled with a telehealth app, shown in the bar chart. Note the delta between consumers overall versus those interested in GLP-1s for weight loss.
The Vitamin Shoppe’s, Eli Lilly’s, and other GLP-1 programs packaged with telehealth support are a point-solution for some consumers’ health — when focused on medical obesity, potentially very powerful as one part of a recipe for people to improve their overall health and well-being to combat the obesity epidemic which also connects to diabesity and heart disease for many patients.
We will continue to monitor all aspects of telehealth, from primary care and prevention to specialty care access, as well as to consumer/retail-driven demand for services like these for the GLP-1s, sexual dysfunction (note Ro’s latest entry into the GLP-1 category expanding beyond its original lifestyle medicines roots). While telehealth can be a solution for addressing health equity and access gaps, some of the retail/consumer-driven programs may exacerbate disparities in access to medicines that can help address public health epidemics. If you want to know more about these issues, check out several of the panels convened at the #ATANexus conference that met this week in Phoenix — LinkedIn, Twitter, and health media covered the meeting in detail.




 Thanks to Feedspot for identifying
Thanks to Feedspot for identifying  Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.
Jane was named as a member of the AHIP 2024 Advisory Board, joining some valued colleagues to prepare for the challenges and opportunities facing health plans, systems, and other industry stakeholders.  Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.
Join Jane at AHIP's annual meeting in Las Vegas: I'll be speaking, moderating a panel, and providing thought leadership on health consumers and bolstering equity, empowerment, and self-care.