Mary Madison, RN, RAC-CT, CDP
Clinical Consultant – Briggs Healthcare
Post-acute care (PAC) represents an important component of the health care delivery system in the United States, with the Medicare fee-for-service program spending more than $57 billion on these services in 2019 (The Medicare Payment Advisory Commission (MedPAC), 2021a). PAC providers include skilled nursing facilities (SNFs), inpatient rehabilitation facilities (IRFs), long-term care hospitals (LTCHs), and home health agencies (HHA) [§ 1899B(a)(2)(A) of the Social Security Act]. It can be provided after an acute care hospitalization as well as for “community entrants” (i.e., patients who do not have a prior acute stay).
Although each type of PAC provider has distinct features and roles within the health care delivery system, the type of services offered in each of these settings can overlap. For example, IRFs and SNFs both treat patients with rehabilitation needs, and SNFs and LTCHs both typically care for patients whose needs are more medical in nature. Although there can be important differences in type and intensity of services patients need, past work has shown that there is also some amount of overlap in patient need in terms of medical condition and level of functional limitations between these settings (Balentine et al., 2018; Barnett et al., 2019; Buntin et al., 2010; Chovanec et al., 2021; Gage et al., 2012; Mallinson et al., 2014; Sharareh et al., 2014).
In 2014, the Improving Medicare Post-Acute Care Transformation (IMPACT) Act was signed into law. A key provision of the IMPACT Act was the development of a technical prototype Unified PAC prospective payment system (PPS) that would set payment for PAC services on the basis of beneficiary clinical characteristics rather than type of provider. The IMPACT Act also required the use of standardized data elements collected across the different PAC settings to be incorporated into and determine payments under the prototype.
In this report, we present the prototype for the Unified PAC PPS and the analyses used to design and calibrate it. We begin by describing the data used in this analysis, including Medicare claims and enrollment data, PAC assessment data, and Medicare cost report data. Because the unit of payment currently varies across the four PAC settings, for the purposes of this work, we defined a PAC “stay” as an individual stay for IRF and LTCH, the total days for which per diem was billed for a SNF stay, and a continuous sequence of HHA episodes. We then present the structure of the prototype—including how it approaches case-mix adjustment and payment weight assignment—and the analyses and results used in developing this framework. Finally, we explore key considerations for unifying PAC payment, such as cost-sharing and value-based payment (VBP).
The 106-page document is found here.
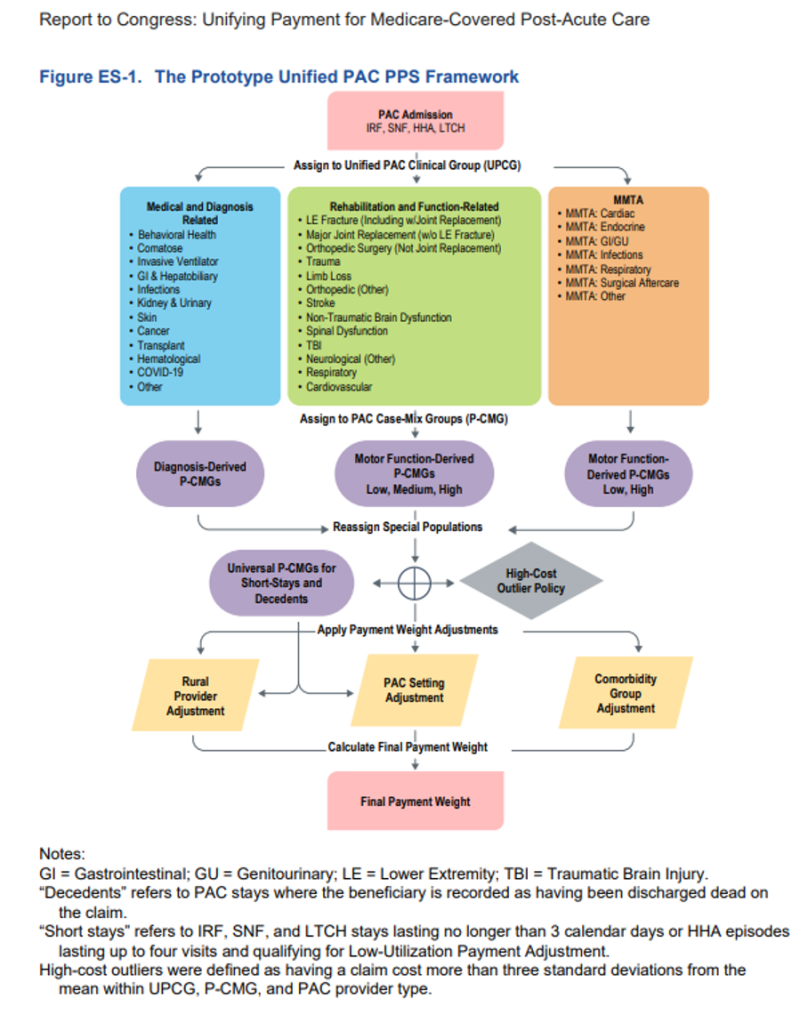
I have not had the time to review this document yet, but I certainly will do so. I encourage you, your team and colleagues to do so as well. We may well be looking at the future of post-acute care reimbursement. Note the verbiage I bolded and underlined in the 3rd paragraph (the report’s Executive Summary) of this blog as well as the figure above I excerpted from the beginning of the report.
