Considerations for States Interested in Applying for the States Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model
The Centers for Medicare & Medicaid Services (CMS) released its latest total cost-of-care model, the States Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model, with the goals of slowing growth in health care costs, improving population health, and advancing health equity (see NASHP’s summary of the model).
Participation will be competitive, with up to eight states selected to participate across three cohorts. States interested in participating in the model were required to submit applications by March 18, 2024, for Cohort 1 or 2 and are required to submit applications by August 12, 2024, for Cohort 3. Specifics required for the applications can be found in the Notice of Funding Opportunity (NOFO).
As states assess their interest and readiness to pursue the model, there are important considerations relating to meeting the requirements of the application (see NASHP’s AHEAD Model Application Assistance Tool) and strategic planning for implementation relating to hospital global budgets. In addition, states are trying to balance the requirements associated with the model and their broader transformation goals. This blog post summarizes both the global budget requirements identified by CMS and additional strategic considerations for states thinking about whether they will pursue the AHEAD Model, to ensure they are well-positioned for application, negotiation, pre-implementation, and implementation.
This blog post was prepared based on a presentation given by Vicki Veltri, NASHP senior policy fellow, and Sule Gerovich, Mathematica senior fellow, on January 11, 2024. It is part of a series highlighting key components of the AHEAD Model for states. See the first blog post in the series covering governance.
AHEAD Model Hospital Global Budget Requirements
Participation in the AHEAD model includes all payer hospital global budgets. By the fourth performance year of the model, 30 percent of Medicare fee-for-service (FFS) revenue of the state (or subregion of a state tied to the model) must be tied to a Medicare hospital global budget. The model also requires Medicaid to establish a hospital global budget for participating hospitals for the first performance year of the model. Finally, by the second performance year, at least one commercial payer must be participating in a hospital global budget. This means there will be three hospital global budgets: Medicare, Medicaid, and commercial.
More about Medicare Hospital Global Budgets
Medicare hospital global budgets are fixed annual budgets for hospital inpatient and outpatient facility services. Under the AHEAD Model, the hospital global budgets will be calculated based on Medicare payments during a baseline period and will include adjustments for inflation, changes in the population served, and changes in the services offered.
Resources from CMS on the Medicare Hospital Global Budget Specifications:
- AHEAD Hospital Global Budget Fact Sheet
- Version 1.0 of the AHEAD Hospital Global Budget Specifications (February 12, 2024)
- CMS-Designated Medicare FFS Hospital Global Budget Methodology Overview Webinar (February 14, 2024) Slides | Transcript | Recording
Medicare Fee-for-Service Hospital Global Budget
CMS will set the methodology for the Medicare FFS hospital global budget. States with existing rate-setting authority and experience may set their own methodologies, subject to CMS approval. Additional states may develop the authority and capacity to set their own Medicare FFS global budget methodology at a later point and submit their methodology to CMS for approval at least 18 months prior to going into effect. Acute care hospitals, critical access hospitals, and rural emergency hospitals (in states with enabling legislation) are eligible to participate in the Medicare FFS hospital global budget. The NOFO includes a high-level overview of the financial methodology. The first version of the financial specifications were released in mid-February (see above), and a final detailed financial methodology will be provided prior to hospitals signing a participation agreement.
Medicaid Hospital Global Budget
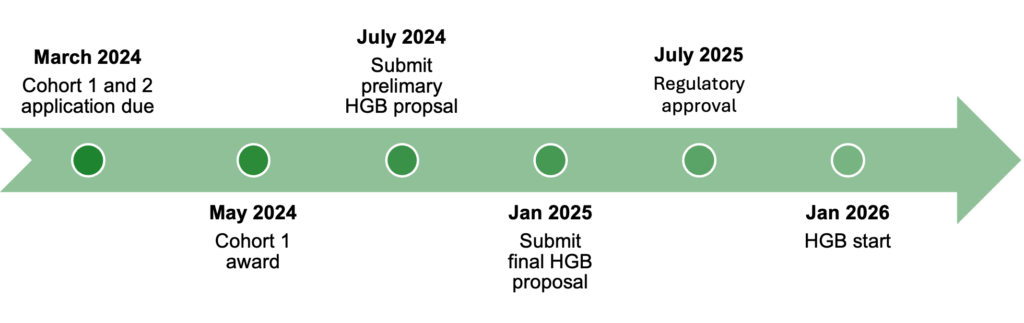
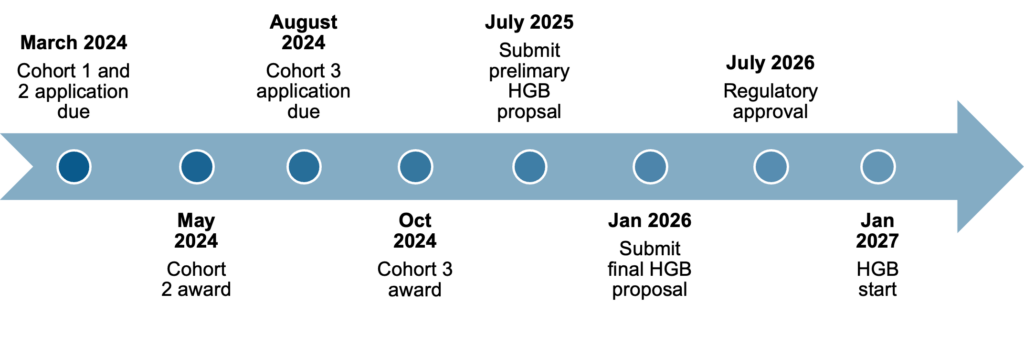
The state Medicaid agency (SMA) is responsible for setting the methodology for the Medicaid hospital global budget, subject to regulatory and CMS approval. States must submit a preliminary Medicaid hospital global budget (HGB) proposal by July 2024 for Cohort 1 and by July 2025 for Cohorts 2 and 3. They must submit a final proposal six months later, followed by final regulatory approval by July the following year (see Figure 1). CMS will review the SMA’s proposed methodologies and necessary Medicaid authorities for implementation. As part of the application, states must include a timeline of activities to develop and implement the methodology, a list of major partner groups to be engaged in the development process, and a plan for recruiting and retaining hospitals.
The Medicaid hospital global budget must be implemented prior to performance year one, but no later than the end of performance year one. States that do not implement by performance year one will receive financial penalties until they meet the requirements; states that do not implement by performance year two may face corrective action up to termination of the agreement.
Figure 1. Milestone Requirements for Medicaid Hospital Global Budgets
Cohort 1 Timelines
Cohort 2 and 3 Timelines
Commercial and/or Medicare Advantage Hospital Global Budget
Participating states will develop the financial methodology, aligned at a high level with the principles laid out by CMS. At least one commercial payer or Medicare Advantage plan must participate in global budgets by performance year two. For this model, commercial payers include marketplace plans (qualified health plans), state employee plans, fully insured plans, and self-funded plans. A state’s lead agency must recruit commercial payers and hospitals to participate.
Hospital Global Budget Key Considerations
The overall goal of hospital global budgets in the AHEAD Model is to incentivize hospitals to focus on population health and health equity, limit avoidable utilization, and control total cost of care by removing FFS incentives and providing financial stability. Patients, hospitals, and payers may be interested in hospital global budgets for multiple reasons (see text box below).
Patients
- Coordinated care
- Primary care and prevention
- Focus on social drivers of health
- Opportunities for patient-centered care and population health efforts
- Better quality and access with strong safety net providers
- Potential benefit enhancements
Hospitals
- Mission alignment and leadership interest
- Stable and predictable revenue
- Operational flexibilities, potential waivers from regulatory requirements
- Transformation incentives (financial, technical assistance, others)
- Primary Care AHEAD, for hospitals that own primary care practices
Payers (Including States)
- Control the growth of hospital cost (40% of total health care dollars)
- Transform health care delivery
- Stabilize safety net hospitals, including rural providers
- Predictable spending
- Operational flexibilities
States and payers may be concerned about pursuing a hospital global budget because hospital prices are already high in many states compared to their costs, and setting global budgets based on current prices may lock in historical inefficiencies and high prices. States and patients may also worry that hospitals on a fixed budget will impose financial pressures that lead to activities such as ceasing certain services to create savings. A hospital global budget itself may not ensure that hospitals invest in the ways the state and payers may have in mind. However, a hospital global budget combined with financial adjustments and accountability targets for transformation, health equity, quality, and population health have the potential to drive hospitals toward making investments that align with the states’ broader goals.
Recruitment: The Opportunity and Challenge of Hospital Global Budgets
Hospital global budgets change the business model of hospitals, requiring investment in transformation. States will be responsible for recruiting hospitals to participate voluntarily in the Medicaid hospital global budget, the Medicare FFS global budget, and the commercial global budget(s).
Hospitals may be worried about how to address factors outside their control and historic scope, including physician practices that may not be owned by a hospital or health system that may continue to have FFS incentives; insufficient or limited access to post-acute care for patients; shortages in the primary care workforce; and social and economic factors, which require significant community engagement. Early engagement, trust building, and being willing to hear and address concerns with hospital leaders (including the board, CEO, and CFO) will be crucial to recruiting participants.
Whether hospitals decide to participate may be predicated on:
- How significant Medicare FFS and Medicaid revenue is for the hospital (see NASHP’s Hospital Cost Tool, which includes information on payer mix over time)
- The extent of the opportunity to reduce hospital utilization (see Mathematica’s tool on potentially avoidable utilization for rural hospitals)
- Whether they already participate in alternative payment models — there may be capacity limitations in navigating multiple models
- The level of trust they have with CMS and the state
While only one commercial plan is required to participate in the model by performance year two, having additional commercial plans participating may assist with hospital recruitment for the Medicare FFS and Medicaid hospital global budgets. States may consider placing incentives on Medicaid managed care plans or use state levers to encourage their participation in Medicaid and/or commercial global budgets. States may also consider engaging employer groups to gauge their interest in the commercial hospital global budget for their plan participants. Employers may be interested in the predictability that comes with hospital global budgets.
Decision Points for States on Medicaid Hospital Global Budgets
Eligibility Requirements
States will be responsible for deciding the eligibility parameters for hospitals, services, and populations that will be included in the Medicaid hospital global budget. While states have some flexibility for exclusions, they may create different incentives and additional validation processes.
- Hospitals: Short-term acute care hospitals, critical access hospitals, and rural emergency hospitals are eligible to participate. Long-term care hospitals and federally owned facilities are not eligible. But states can consider including other specialized hospitals to address their unique priorities.
- Services: At a minimum, hospital global budgets will be required to include inpatient, outpatient, and emergency department facility services. States will decide whether to include other professionals and/or services in the hospital global budget.
- Populations: States and CMS may negotiate excluding certain populations from the hospital global budget.
Methodology Design
States are responsible for designing the Medicaid hospital global budget methodology that needs to be approved by CMS. As they do so, they may consider overall alignment with the existing system and impact on the overall Medicaid and state budgets. To ease administrative burden on providers, states will likely want to align with the Medicare budget methodology as much as possible.
- Managed care: States with managed care arrangements will consider the role of Medicaid managed care organizations in the model, how the global budget may affect their rates, and how much risk will reside with them. Some decisions can be left to negotiation between plans and hospitals, or states can establish the model directly.
- Authority mechanisms: States will consider what mechanisms and authority are needed for implementation. The CMS Innovation Center will approve the Medicaid hospital global budget methodology and the Center for Medicaid and CHIP Services will need to approve state plan amendments, Section 1115 demonstration waivers, and/or other needed authorities. In some cases, states may also need legislative action to proceed.
- Adjustments: States may consider what adjustments to include to ensure quality while accounting for changes in services and populations. States will aim to balance maintaining quality, allowing for competition, and facilitating flexibility. States can request flexibility on quality measures as part of the model. Ultimately, states will likely aim for fewer unnecessary services and more necessary services for the community.
- Monitoring and accountability: Hospital global budgets provide fixed revenue, which can incentivize providing fewer services. Therefore, strong monitoring, accountability, and incentives are needed to ensure access and quality of necessary services.
- Geographic attribution: States will design beneficiary attribution models, to include geographic attribution, facilitation with calculating the budgets, accounting for membership changes, and performance measures.
- Payment: States will decide on a payment approach, which may include paying prospectively on a monthly basis instead of paying individual claims. Alternatively, states may continue to pay through a virtual budget via claims and a reconciliation to the budget at the end of the period.
Next Steps
NASHP and Mathematica are collaborating on a series of state-only conversations for states interested in AHEAD. The first virtual meeting on December 19, 2023, focused on governance, as described in the first blog post of the series. The second virtual meeting was held on January 11, 2024, and focused on hospital global budgets, as described here. The third virtual meeting was held on January 18, 2024, and focused on primary care, which will be described in a future blog post. A fourth virtual meeting was held on February 22, 2024, to review the first version of the AHEAD Hospital Global Budget Specifications, which were released by CMS on February 15, 2024 (access the slides; additional analysis from NASHP is forthcoming). NASHP and Mathematica will hold additional virtual meetings in 2024. Participants will have the opportunity to hear from and engage with experts and discuss with their peers in other states key model issues and consideration