Rates of maternal mortality in the U.S. remain consistently high, with most deaths occurring postpartum. There are significant racial disparities among those affected by maternal mortality. Non-Hispanic Black women disproportionately face adverse maternal health outcomes. Pregnancy-related mortality rates among Black women are two to three times the rate for women of other races. Georgia’s efforts illustrate one state’s approach to addressing maternal morbidity and mortality rates by strengthening access to maternal health services while maintaining long-term financial sustainability.
Access to quality health services is essential as most preventable pregnancy-related deaths are attributed to mental health and cardiac and coronary conditions. As the payor of over 40 percent of U.S. births, Medicaid and the Children’s Health Insurance Program (CHIP) are critical in addressing this maternal health concern. Assuring postpartum coverage may help address this public health issue by providing preventive care and chronic condition management to low-income pregnant and postpartum women.
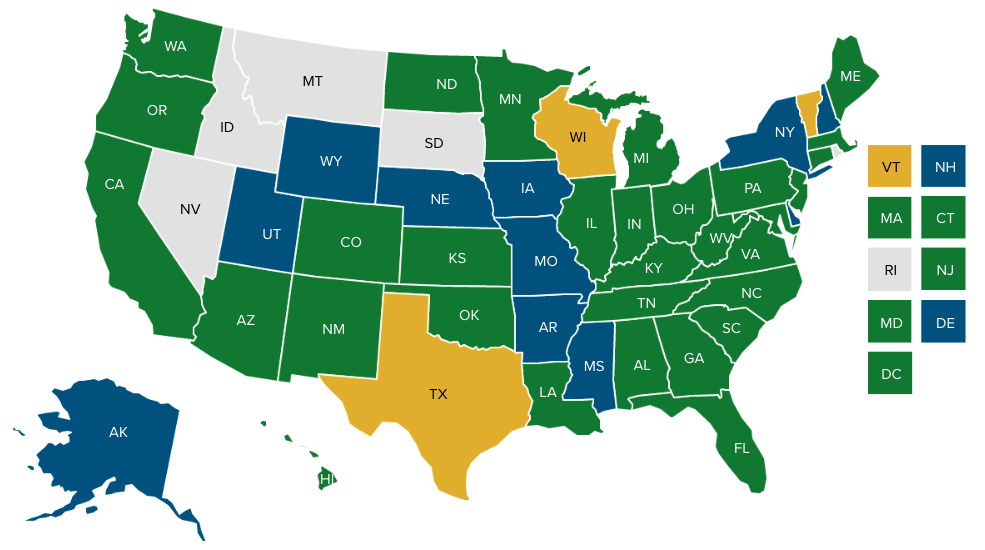
States are increasingly exploring and implementing Medicaid postpartum coverage to improve maternal health outcomes. In November 2022, Georgia joined 29 states, including Washington, DC, to implement a 12-month extension of Medicaid postpartum coverage. NASHP tracks state efforts to extend Medicaid postpartum coverage.
In October 2022, the Centers for Medicare & Medicaid Services (CMS) approved two Georgia state plan amendments (SPAs) to increase coverage of postpartum services to 12 months. The first SPA grants continuous coverage for Medicaid-eligible pregnant and postpartum people, whereas the second SPA provides the same benefits but for pregnant or postpartum CHIP members who do not qualify for Medicaid. The SPAs continue implementing services outlined in Georgia’s Postpartum Extension Demonstration that went into effect in July 2021 for five years. The demonstration was authorized by a section 1115(a) waiver, which increased health care coverage from 60 days to six months postpartum. The demonstration allowed postpartum women with an income of up to 220 percent of the federal poverty level to receive extended benefits, continuous coverage, and suspended redetermination. The postpartum extension authorized under the SPAs allows the state to recommence these activities through 12 months postpartum. This policy change will be permanent, per the Consolidated Appropriations Act of 2023.
Extending Postpartum Coverage through the American Rescue Plan Act
The American Rescue Plan Act of 2021 (ARPA) grants states the 12-month extension option through a state plan amendment. Beginning April 1, 2022, ARPA allows states to opt-in to provide 12-month postpartum coverage to eligible Medicaid and CHIP recipients.
Once a state receives federal approval to extend postpartum coverage through the ARPA option, that extension is made permanent. This option was made possible by the Consolidated Appropriations Act of 2023. The law promotes closing the coverage gap, creating better health outcomes for uninsured reproductive-age people. Furthermore, states can utilize this opportunity to provide continuity of care for enrollees who could lose coverage after the end of the federal COVID-19 public health emergency declaration rolls back the Medicaid continuous coverage requirement.
Medicaid-enrolled postpartum people benefiting from Georgia’s recent postpartum coverage extension will be enrolled in Medicaid-managed care plans. Georgia’s Department of Community Health designed the Resource Mothers Outreach program to prioritize care utilization and coordination of care. Administered by care management organizations, Resource Mothers are trained paraprofessionals supervised by nurse managers. In the program, pregnant or postpartum Medicaid and CHIP beneficiaries receive:
- Preventive health services or family planning consultations
- Support for appointments and medication compliance
- Health education to support behavioral changes
- Help with the coordination of social services and community resources
Georgia’s efforts to address maternal mortality, partly through Medicaid postpartum coverage extension, build upon previous legislative action to address this public health concern. In 2013, the Georgia General Assembly authorized a maternal mortality review committee (MMRC) to end preventable maternal deaths through data collection, case review, and analysis. The MMRC found that Medicaid enrollees accounted for 68 percent of pregnancy-related postpartum deaths, and over 60 percent were preventable. The MMRC also found that non-Hispanic Black women experienced preventable deaths at above twice the rate of non-Hispanic White women, accounting for 48.6 deaths per 100,000 births. The MMRC strongly recommended case management, coverage extension, and increased access to family planning and contraception services in response to these findings. The MMRC’s findings led to the passage of Senate Bill 338, which authorized Medicaid coverage for lactation and postpartum services up to one year after pregnancy ends and directed the Department of Community Health to submit the SPA to CMS. This provision also expanded care for individuals after experiencing a miscarriage or abortion. These policy changes can potentially support advancements in the state’s maternal health landscape.
Health care innovation and quality improvement are key to combating the maternal health crisis, particularly disparities in maternal mortality and morbidity. Georgia’s efforts to extend Medicaid postpartum coverage exemplify how federal and state policies can strengthen systems supporting maternal health care. NASHP continues to support state efforts by highlighting equitable policy strategies in maternal health.
Acknowledgements
Maureen Johnson was a 2022 NASHP Emerging Leader of Color Fellow. As part of this fellowship, she was paired with Georgia’s Medicaid officials to learn and support the state’s maternal health efforts. The ELC Fellowship provides professional development to aspiring state policy leaders.
This case study is a publication of the National Academy for State Health Policy (NASHP). This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under the Supporting Maternal and Child Health Innovation in States Grant No. U1XMC31658; $398,953. This information, content, and conclusions are those of the authors’ and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS, or the U.S. government.