States that expanded Medicaid coverage under the Affordable Care Act (ACA) saw a significant decrease in Medicare-financed hospitalizations after initiation of dialysis treatment for patients suffering from kidney disease compared to nonexpansion states, according to a study in JAMA Health Forum.
The study states that among Medicare beneficiaries aged 19 to 64 years with incident kidney failure, Medicaid expansion was associated with a significant decrease in mortality rates 12 months after dialysis initiation.
Researchers with Brown University also found that Medicaid expansion decreased Medicare-financed hospitalizations for patients three months after the start of dialysis. In addition, there was a decrease in the number of hospital days at three and six months after the beginning of dialysis.
Kevin H. Nguyen, PhD, of the department of health services, policy, and practice at Brown University School of Public Health, and the study’s corresponding author, tells Fierce Healthcare that “for policymakers, the key lesson is that the ACA’s Medicaid expansion may have favorable spillovers to the Medicare program in the form of reduced spending on hospitalizations, which is the largest source of expenditures in Medicare. I would also note another key finding is that, among adults aged 19-64 with kidney failure, Medicaid expansion was associated with fewer hospitalizations in the first year after initiating dialysis, which is a particularly high-risk period for people with kidney failure.”
Researchers examined the results from the different approaches to Medicaid expansion up to five years after that expansion among individuals aged 19 to 64 who were covered by Medicare Part A and who initiated dialysis between Dec. 31, 2018, and Jan. 1, 2020.
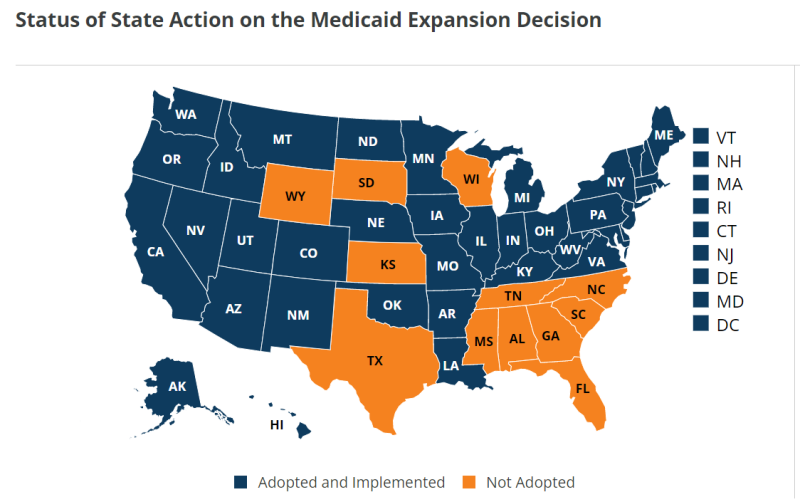
Data were taken from 188,671 adults, 97,071 living in Medicaid expansion states and 91,600 living in nonexpansion states. Medicaid expansion was associated with a significant decrease in Medicare-financed hospitalizations, and hospitalizations per 100 patient-years, with a relative reduction of 8% for both outcomes.
In addition, Medicaid expansion was associated with a 2.58 percentage point increase in dual Medicare and Medicaid coverage at 91 days after initiation of dialysis, particularly for Hispanic or Latino patients with kidney failure. Researchers saw a 1.65 percentage point increase in arteriovenous fistula (AVF) or graft at initiation.
“Although there were no significant changes in the receipt of predialysis nephrology care, rates of dialysis initiation with an AVF or graft present among patients undergoing hemodialysis significantly increased in states that expanded Medicaid,” the study states.
The researchers note that before the ACA, in most states, individuals aged 19 to 64 on Social Security Disability Insurance (SSDI) could only receive supplemental Medicaid coverage if they qualified for means-tested Social Security income disability.
“The ACA expanded access to Medicaid for SSDI recipients aged 19 to 64 years with low household incomes in addition to increasing Medicaid participation among those already eligible for coverage because of publicity, enrollment efforts, and other factors, which is sometimes referred to as the woodwork or welcome mat effect,” the study states. “Recent evidence suggests that Medicaid expansion was associated with increases in dual Medicare and Medicaid coverage for older adults with low household incomes and individuals with disabilities. This study supports these estimates, suggesting that patients with incident kidney failure had pronounced increases in dual Medicare and Medicaid coverage after expansion.”
The authors note that some policymakers believed Medicaid expansion would lead to either increased hospitalization or no changes in hospitalizations.
“Findings of the present study, which used national data and focused on a high-need and clinically complex patient population, suggest that Medicaid expansion was associated with significant reductions in all-cause and infection-related hospitalizations,” the study states. “These results align with past work finding that, among Medicare beneficiaries, particularly those with chronic conditions, lower cost-sharing may increase access to effective outpatient care and generate offsetting reductions in acute hospitalizations.”
Data were obtained from the Renal Management Information System’s End Stage Renal Disease Medical Evidence Report, which includes all patients undergoing outpatient maintenance dialysis regardless of treatment modality, citizenship status or health insurance coverage. Researchers also used claims data from the Medicare Provider Analysis and Review. Data were analyzed from January to August 2022.
Authors argue that spillover occurred from expanded Medicaid into Medicare reduced hospitalizations, the largest cost factor in Medicare. In addition, hospitalization rates are higher among people with kidney failure, and Medicaid expansion helped tamp down those costs for people battling that disease in the 19- to 64-year-old age group.
“The relative 8% decreases associated with Medicaid expansion were large in magnitude considering the secular trend between 2007 and 2016 was a 15% decline,” the study states. “This finding is critical because reducing hospitalizations among the population with kidney failure is a clinical and policy priority, including public reporting on hospitalization rates for dialysis facilities. Furthermore, Medicare is the primary payer for care among people with kidney failure, and hospitalizations account for approximately 40% of Medicare expenditures for patients undergoing dialysis. Significant decreases in 1-year mortality rates associated with Medicaid expansion support past findings and extend this work to Medicare beneficiaries initiating dialysis treatment.”