During the COVID-19 public health emergency (PHE), states received approval from the federal government to implement Appendix K amendments to 1915(c) home-and community-based waivers and 1115 demonstration waivers to ensure that Medicaid beneficiaries were able to receive needed services during the pandemic. With the end of the COVID-19 PHE declaration on May 11, 2023, states must decide if and what types of flexibilities will be sustained long-term.
NASHP fielded a 50-state survey and scanned state websites examining which of nine flexibilities the state planned to sustain post-PHE in at least one of the state’s aging/physical disability waivers. We identified the plans of 47 states and Washington, DC and found that 41 states and DC planned to sustain at least one flexibility post-PHE through waiver amendments, legislation, and/or regulations:
- Allow Medicaid payment to parents, spouses, and/or legally responsible individuals — at least 23 states
- Increase Medicaid payment rates for direct care workers, such as personal care aides, home care aides, and/or certified nursing assistants — at least 22 states
- Add or expand assistive technology services, such as expanding definitions of assistive technology to include internet and remote support, developing assistive technology pilot programs, or raising spending limit caps — at least 16 states
- Allow remote or virtual options to conduct evaluations, assessments, and person-centered service planning meetings — at least 16 states
- Add electronic service delivery methods for services, such as personal care services that only require verbal cueing, in-home habilitation, or training and support — at least 15 states
- Add an electronic method of signing required documents — at least 14 states
- Add or expand home-delivered meals — at least 10 states
- Expand access to self-direction in addition to flexibilities on allowing payment to parents, spouses, relatives, and/or legally responsible persons — at least 4 states
- Increase services for family caregivers, including respite services and adult day health services — at least 5 states
Appendix K and emergency waivers created a lasting impact in many states on home and community-based services for Medicaid beneficiaries who are older and/or have disabilities that will extend past the COVID-19 pandemic emergency. More than half of states (33) plan to sustain flexibilities affecting payment to family caregivers and/or to professional caregivers.
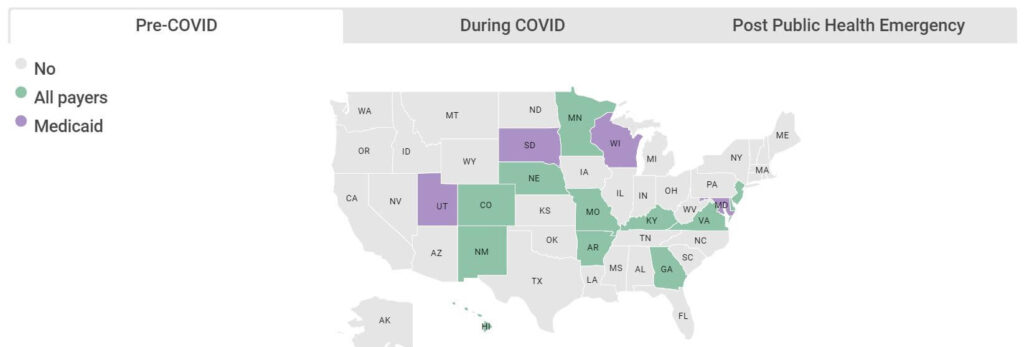
More information about planned sustained flexibilities can be viewed in the map and chart below. Information was collected between May 9 and June 23, 2023.
This work was supported by a generous grant from The John A. Hartford Foundation.