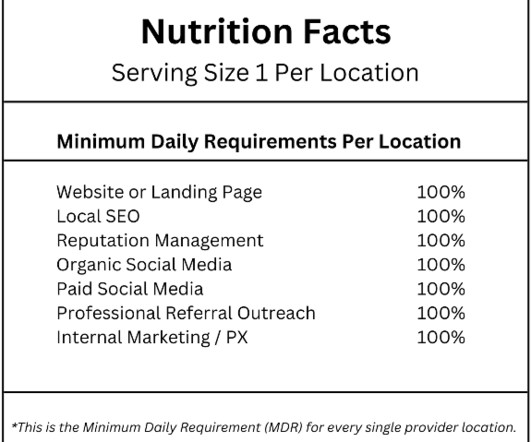
Multilocation Healthcare Marketing: Minimum Daily Requirements
Healthcare Success
OCTOBER 30, 2023
Do you want to position your healthcare products and services where your target audience actively seeks them? Reputation Management High-quality reviews and ratings are key influencers for patients. This requires ongoing monitoring, reviewing, and responding to ensure a positive online reputation.











Let's personalize your content