Mary Madison, RN, RAC-CT, CDP
Clinical Consultant – Briggs Healthcare
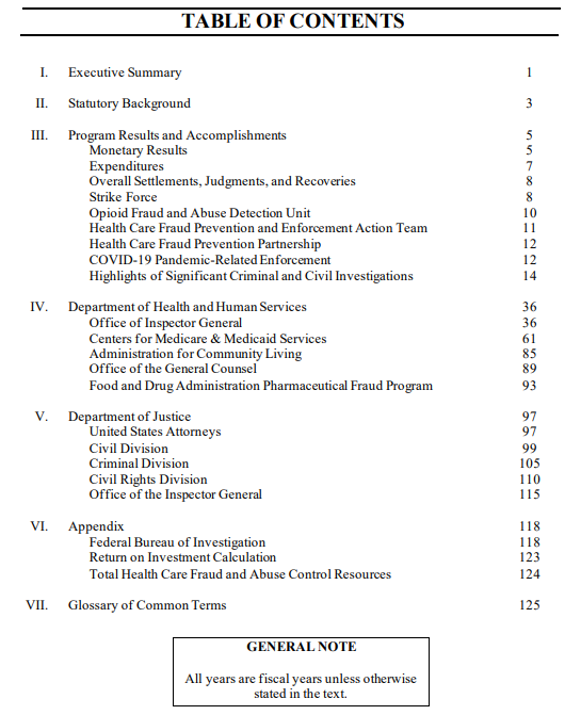
The national Health Care Fraud and Abuse Control (HCFAC) Program is celebrating its 25th year of operation and continued success in identifying and prosecuting the most egregious instances of health care fraud, preventing future fraud and abuse, and protecting program beneficiaries. The HCFAC Program is designed to coordinate Federal, State and local law enforcement activities with respect to health care fraud and abuse. The program is under the joint direction of the Attorney General and the Secretary of the Department of Health and Human Services, acting through HHS-OIG. OIG publishes the Health Care Fraud and Abuse Control Program Report for Fiscal Year 2021.
During Fiscal Year (FY) 2021, the Federal Government won or negotiated more than $5 billion in health care fraud judgments and settlements, in addition to other health care administrative impositions. Because of these efforts, as well as those of preceding years, almost $1.9 billion was returned to the Federal Government or paid to private persons in FY 2021.
You’ll find the 129-page report here.
In FY 2021, the Department of Justice (DOJ) opened 831 new criminal health care fraud investigations. Federal prosecutors filed criminal charges in 462 cases involving 741 defendants. A total of 312 defendants were convicted of health care fraud related crimes during the year. Also, in FY 2021, DOJ opened 805 new civil health care fraud investigations and had 1,432 civil health care fraud matters pending at the end of the fiscal year. Federal Bureau of Investigation (FBI) investigative efforts resulted in over 559 operational disruptions of criminal fraud organizations and the dismantlement of the criminal hierarchy of more than 107 health care fraud criminal enterprises.
In FY 2021, investigations conducted by HHS’s Office of Inspector General (HHS-OIG) resulted in 504 criminal actions against individuals or entities that engaged in crimes related to Medicare and Medicaid, and 669 civil actions, which include false claims and unjust-enrichment lawsuits filed in federal district court, and civil monetary penalty (CMP) settlements. HHS-OIG also excluded 1,689 individuals and entities from participation in Medicare, Medicaid, and other federal health care programs. Among these were exclusions based on criminal convictions for crimes related to Medicare and Medicaid (569) or to other health care programs (267), for beneficiary abuse or neglect (145), and as a result of state health care licensure revocations (536).
Sequestration of mandatory funding generally results in DOJ, FBI, HHS, and HHS-OIG having fewer resources to fight fraud and abuse of Medicare, Medicaid, and other health care programs. Due to sequester suspension, no funds were sequestered from the HCFAC program in FY 2021. However, a combined total of $150.6 million in mandatory funds have been sequestered in the past nine years. Including funds sequestered from the FBI ($70.0 million in the past nine years), $220.6 million has been sequestered from mandatory HCFAC funds since FY 2013.
