Family caregivers across the nation have emphasized to the RAISE Act Family Caregiving Council that what they often need is respite care — that is, services that provide caregivers time off to attend to their own needs and obtain relief from the ongoing demands of care work. In this context, adult day services were frequently mentioned, too. However, family caregivers often have difficulties with accessing this care, especially for those caregivers who are providing skilled care and/or caring for people with serious mental and behavioral conditions. With Medicaid as the major public payer of respite and adult day services, states have a significant role in determining how individuals may be able to access such services. To better understand Medicaid respite care and adult day services policies in each state, NASHP recently conducted 50-state research and published the findings in a series of interactive maps.
Findings
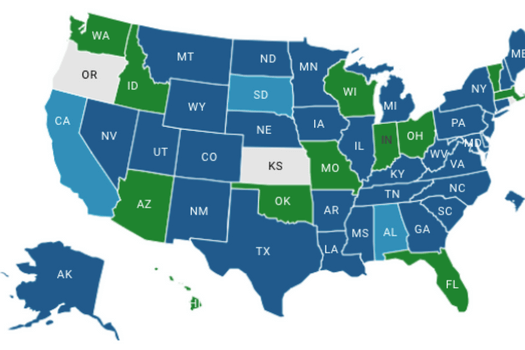
Most states cover respite care and adult day services in their Medicaid home and community-based waivers and state plan authorities, but the majority of states place a limit on the amount of respite services covered. Respite covered under state Medicaid programs for children with special health care needs ranges from 7 days (Florida) to 180 days (Minnesota) per service year. For older adults and adults with physical disabilities, the range of respite covered under Medicaid spans 9 days (Tennessee) to 50 days (Arkansas) per service year, with a median of 29 days per service year. However, a minority of states allows for respite care coverage under Medicaid based on an assessed need in an individual’s service plan to determine service amounts. For more information, view this interactive map. Also included are detailed charts on each state’s respite and adult day waiver services for older adults and adults with physical disabilities and for children and youth with special health care needs.
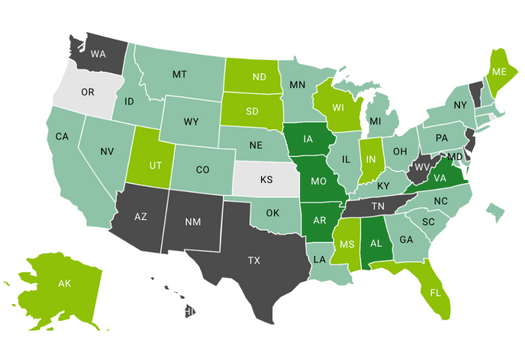
Although most states’ Medicaid programs cover respite care and adult day services, anticipated expenditures are relatively low compared to overall spend on home and community-based services. In order to better understand state spending on these services, we reviewed state cost estimates located in Appendix J within each Medicaid 1915(c) waiver application. We found that states that offer respite care under a Medicaid 1915(c) home and community-based waiver spent a median percentage of 0.49% of the total waiver expenditure, with 24 states allocating less than 2%, nine states between 2.01-10% in at least one waiver, and five states with over 10+% in at least one waiver. For states that offer adult day within a Medicaid 1915(c) home and community-based waiver, the median percentage of adult day funding allocated is only 1.01% of the total waiver expenditure, with 20 states allocating less than 2%, 13 states between 2.01-10% in at least one waiver, and five states with over 10+% in at least one waiver. There are a few exceptions to this; most notably Missouri’s Aged and Disabled Waiver (51%) and Iowa’s HCBS Health and Disability Waiver (34%). For adult day services, a few states have waivers solely dedicated to the service, such as Louisiana’s Adult Day Health Care (ADHC) waiver and Missouri’s Adult Day Care waiver.
While some states cover respite care through other regulatory and program mechanisms such as SPAs, 1115 waivers, the Lifespan Respite Care Program, and the National Family Caregiver Support Program, NASHP used for this analysis these 1915(c) Appendix J cost estimates because timely, accurate respite care and adult day services claims data for all 50-states are not available. For more information, view this interactive map and chart.
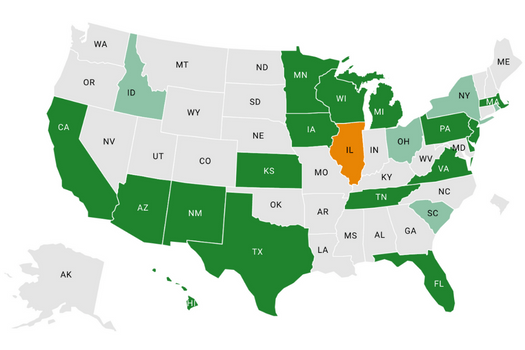
Nearly half of states use Medicaid managed long-term services and supports (MLTSS) to provide services for older adults and adults with physical disabilities — and while all these states cover respite and adult day services, some give managed care organizations greater flexibility to provide these services. Managed care plans are generally required to provide benefits consistent with state plan coverage but have the flexibility to provide benefits beyond minimum requirements. Most waiver applications had greater service-specific information compared to managed care contracts. However, by reviewing states’ managed care contracts, state requests for applications, and managed care policy manuals, NASHP found some state examples of managed care organizations’ (MCOs) flexibility to expand respite coverage. Two states (Kansas and Texas) use contractual language with MCOs to expand respite service coverage and eligibility as a value-added benefit not typically included in a state’s Medicaid waiver program. Four states (Florida, Iowa, Michigan, and Texas) use contractual language to give MCOs the flexibility to increase respite care service limits to exceed those found in the states’ Medicaid waivers. For more information, view this interactive map. For a detailed inventory of each MLTSS state’s respite and adult day services, along with links to managed care contracts, state requests for applications, and managed care policy manuals, view this chart.
Conclusion
With the COVID-19 pandemic and the critical shortage of direct care workers who provide care, there is now a heightened reliance on family caregivers who often report that what they need is a break. This crisis of care is falling on state policymakers who are looking for solutions. The 50-state research scans and maps show that coverage for respite care and adult day services vary greatly by Medicaid waiver and MLTSS programs. These policies have a direct effect on caregivers of Medicaid beneficiaries. As states consider workforce challenges, considering how to better support family caregivers is one strategy that is important in identifying opportunities to extend care at the community level.
Acknowledgements
This project was made possible by support from the Administration for Community Living (ACL), U.S. Department of Health and Human Services (HHS) and The John A. Hartford Foundation as part of a financial assistance award totaling $942,520 with 75 percentage funded by ACL/HHS and $312,845 amount and 25 percentage funded by non-government source(s). The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by ACL/HHS, or the U.S. Government.