Mary Madison, RN, RAC-CT, CDP
Clinical Consultant – Briggs Healthcare
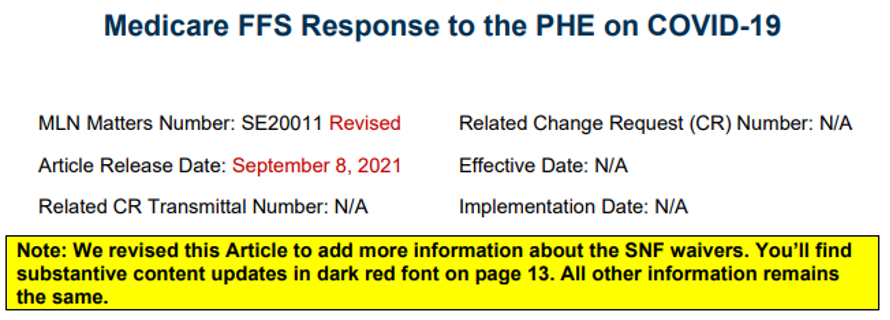
CMS issued this revised SE20011 (19 pages) on September 8, 2021.
SNF Qualifying Hospital Stay (QHS) and Benefit Period Waivers – Provider Information
CMS recognizes that disruptions arising from a PHE can affect coverage under the SNF benefit:
- Prevent a patient from having the 3-day inpatient QHS
- Disrupt the process of ending the patient’s current benefit period and renewing their benefits
The emergency SNF QHS and benefit period requirements under Section 1812(f) of the Social Security Act help restore SNF coverage that patients affected by the emergency would be entitled to under normal circumstances. By contrast, these emergency measures don’t waive or change any other existing requirements for SNF coverage under Part A such as the SNF level of care criteria, which remain in effect under the emergency.
Using the authority under Section 1812(f) of the Social Security Act, CMS doesn’t require a 3-day prior hospitalization for coverage of a SNF stay, which provides temporary emergency coverage of SNF services (including SNF-level swing-bed services in rural hospitals and CAHs) without a QHS, for those people who experience dislocations, or are otherwise affected by COVID-19. At the same time, we’re monitoring for any SNF admissions under Section 1812(f) that don’t meet the SNF level of care criteria (which, as noted above, remain in effect during the emergency), and we’ll take appropriate administrative action in any instances that we find. See SNF Billing Reference for more information on SNF eligibility and coverage requirements.
Also, for certain patients who recently exhausted their SNF benefits, the waiver authorizes a one-time renewal of benefits for an added 100 days of Part A SNF coverage without first having to start a new benefit period (this waiver will apply only for those patients who have been delayed or prevented by the emergency itself from commencing or completing the process of ending their current benefit period and renewing their SNF benefits that would have occurred under normal circumstances).
For the QHS waiver:
- All patients qualify, regardless of whether they’ve SNF benefit days remaining
- The patient’s status of being “affected by the emergency” exists nationwide under the current PHE. (You don’t need to verify individual cases.)
In contrast, for the Benefit Period Waiver:
- Patients who exhaust their SNF benefits can get a renewal of SNF benefits under the waiver except in one particular scenario: that is, those patients who are receiving ongoing skilled care in a SNF that is unrelated to the emergency, as discussed below. To qualify for the benefit period waiver, a patient’s continued receipt of skilled care in the SNF must in some way be related to the PHE. One example would be when a patient who had been receiving daily skilled therapy, then develops COVID-19 and requires a respirator and a feeding tube. We would also note that patients who don’t themselves have a COVID-19 diagnosis may nevertheless be affected by the PHE (for example, when disruptions from the PHE cause delays in obtaining treatment for another condition).
- Wouldn’t apply to those patients who are receiving ongoing skilled care in the SNF that is unrelated to the emergency – a scenario that would have the effect of prolonging the current benefit period and precluding a benefit period renewal even under normal circumstances. For example, if the patient has a continued skilled care need (such as a feeding tube) that is unrelated to the COVID-19 emergency, then the patient can’t renew his or her SNF benefits under the Section 1812(f) waiver as it’s this continued skilled care in the SNF rather than the emergency that is preventing the patient from beginning the 60 day “wellness period.”
- In making determinations, a SNF resident’s ongoing skilled care is considered to be emergency-related unless it is altogether unaffected by the COVID-19 emergency itself (that is, the patient is receiving the very same course of treatment as if the emergency had never occurred). This determination basically involves comparing the course of treatment that the patient has actually gotten to what would have been provided absent the emergency. Unless the two are exactly the same, the provider would determine that the treatment has been affected by and related to the emergency.
- Providers should use the above criteria in determining when to document on the claim that the patient meets the requirement for the waiver.
Keep reading this MLN Matters for additional information. I’ve stopped excerpting the above about a third of the way down on page 14, so you’ll need to finish reading the remaining pages to get all the information. There isn’t any additional new information beyond what I’ve provided, including the red font, but all the information is important to your team, particularly your billers.
