Value-based insurance design (VBID) is a term used to describe health plan benefit design that encourages use of high-value services by lowering or eliminating employee cost sharing obligations for those services and potentially increasing cost sharing on lower-value services. VBID programs are generally voluntary.
According to the University of Michigan’s Center for Value Based Insurance Design, the intent is to encourage use of high-value services to motivate health and to reduce the use of low-value services that increase costs for health plans and beneficiaries. Several states incorporate VBID into their state employee plans. Connecticut and Minnesota have longstanding VBID programs.
Connecticut
Connecticut started its VBID program, the Health Enhancement Program (HEP), in 2011 as the result of a collective bargaining agreement reached with labor to address a deep budget deficit. The goals of the program included improving the health of employees and family members enrolled in the state plan or its Partnership Plan by connecting them to primary care for preventive screenings and management of chronic conditions and to save long-term costs for the state plan.
The HEP applies to state employees, retirees under 65, and municipal employees and retirees participating in the state’s Partnership Plan. The program is voluntary, but those who enroll and meet the HEP requirements are exempt from an additional $100 per month in premium and the elimination of deductibles that could save an individual up to $350 per year and a family up to $1,400 per year.
The program requires that enrollees, based on their ages, make regular visits for certain preventive screening and exams, as outlined in the chart below.
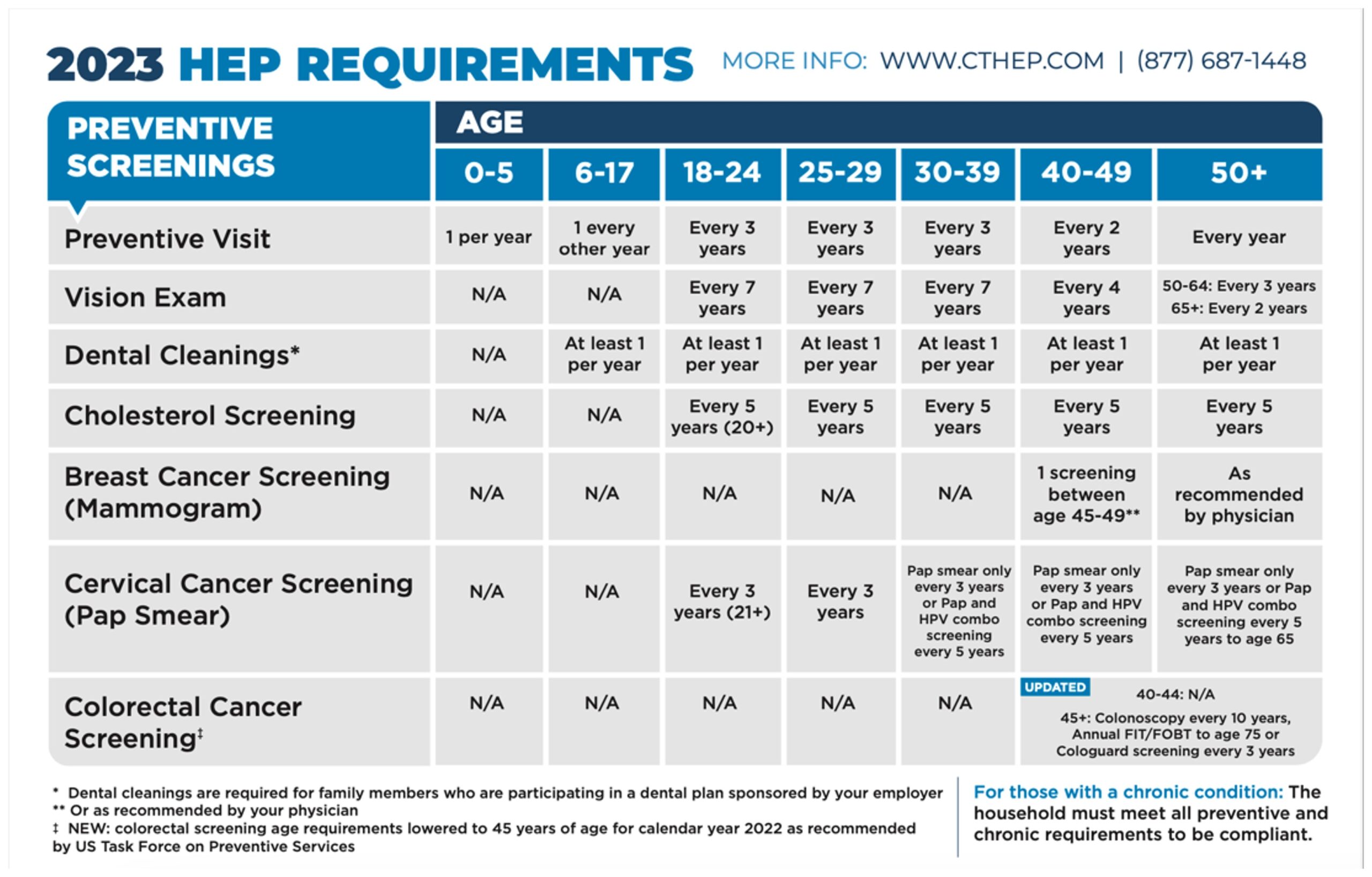
Children in HEP meet requirements through child well-visits and screenings.
Besides the screenings identified above, the HEP requires that enrollees with any of six chronic conditions — asthma, COPD, diabetes (Types 1 and 2), coronary artery disease (CAD), hyperlipidemia (high cholesterol), and hypertension (high blood pressure) — engage in education about their condition. Enrollees can meet educational requirements online or through consultation with a nurse. Enrollees’ chronic conditions are identified through claims data.
Enrollees in the HEP also pay lower or no copays for maintenance medications for the identified chronic conditions. Enrollees with either Type 1 or Type 2 diabetes pay nothing out of pocket for medications or supplies to treat their diabetes. The HEP waives copays for enrollees for visits related to all the above chronic conditions.
The state measures enrollee compliance on a calendar year basis. Employees have access to a portal through which they can review their compliance with requirements and complete educational requirements regarding their chronic conditions. The site also allows employees to request a waiver, if warranted. The state works with a vendor to review compliance with requirements based on claims data. The plan notifies participants if they have not fulfilled requirements during the calendar year to encourage compliance. Participants may be disenrolled from the program, but not before being provided opportunities to come into compliance with HEP requirements.
The compliance rate has been 98 percent for those enrolled in the program each year that compliance has been measured. Compliance was suspended during the COVID-19 pandemic. Now the state is working to embed the financial incentives and disincentives into total cost of care primary care reforms and value-based arrangements with providers.
The state has also been monitoring the development and availability of prescription drugs to address obesity. The state of Connecticut began an engagement on July 1, 2023, with a Connecticut startup, Intellihealth, to manage a comprehensive obesity program that will include the use of prescription drugs.
Minnesota
Minnesota started its VBID program in January 2018. The program is called Advantage Value for Diabetes and is offered by the State Employee Group Insurance Program (SEGIP) as part of the state’s Advantage Health Plan. Minnesota offers Advantage Value for Diabetes to employees, dependents, and former employees with continued coverage. The goal is to help members diagnosed with Type 1 or Type 2 diabetes to effectively maintain their condition, thereby reducing the risk of complications that can be costly to the plan and detrimental to quality of life for the member.
Minnesota identified diabetes as a significant driver of its health spending for both the plan and its members. By lowering cost-sharing for high-value services related to diabetes, the state incentivizes its members to seek regular physician and dietician office visits and retinal eye exams and to regularly monitor their labs. In addition, the diabetes-specific benefit design includes significantly reduced out-of-pocket costs for diabetes-related medical supplies such as insulin pumps and continuous blood glucose monitors.
The cost-sharing reduction for a given service depends on the cost level of the primary care clinic designated by the member. Over 90 percent of SEGIP’s membership is enrolled in cost levels 1 and 2, meaning that all qualifying diabetes services under the program are free to the vast majority of SEGIP members with a diabetes diagnosis.
Out-of-pocket medical costs for Advantage Value for Diabetes in 2023
The benefits below are for care primarily for diabetes through your primary care clinic or referred in-network provider (call your health plan to determine if you need a referral). All care not primarily related to diabetes is covered under the standard Minnesota Advantage Health Plan benefits.
| Eligible Medical Services | Cost Level 1 You Pay | Cost Level 2 You Pay | Cost Level 3 You Pay | Cost Level 4 You Pay |
|---|---|---|---|---|
| Physician Office Visits | $0 copay, deductible waived | $0 copay, deductible waived | $35 copay, deductible waived | $55 copay, deductible waived |
| Dietitian Office Visits | $0 copay, deductible waived | $0 copay, deductible waived | $35 copay, deductible waived | $55 copay, deductible waived |
| Diabetic Retinal Eye Exams | $0 copay, deductible waived | $0 copay, deductible waived | $0 copay, deductible waived | $0 copay, deductible waived |
| Labs: LDL Panel, Urine Protein test, Glucose test, Hemoglobin A1C | 0% coinsurance, deductible waived | 0% coinsurance, deductible waived | 0% coinsurance, deductible waived | 0% coinsurance, deductible waived |
| Diabetic Testing Supplies (including covered insulin pumps, continuous glucose monitors) | 10% coinsurance, deductible waived | 10% coinsurance, deductible waived | 10% coinsurance,, deductible waived | 10% coinsurance, deductible waived |
| Medication Therapy Management (Pharmacist Consults) | $0, copay, deductible waived | $0 copay, deductible waived | $0, copay. deductible waived | $0, copay, deductible waived |
Source: https://mn.gov/mmb-stat/segip/diabetic-mtm-management/vbid-benefit-description.pdf
Recognizing that adherence to prescription drug regimens is a vital component of effective chronic condition management, Minnesota also reduced out-of-pocket costs for certain prescription medications.
Out-of-pocket pharmacy costs for Advantage Value for Diabetes in 2023
These out-of-pocket savings apply for medications purchased through in-network pharmacies. These medications may be purchased through retail pharmacy locations, mail, and other specialty services outlined by CVS Caremark.
| Eligible Drugs/Supplies | You Pay |
|---|---|
| Diabetes medications | Copay: $0 tier 1 / $20 tier 2 / $35 tier 3 |
| Hypertensive (blood pressure) medications | Copay: $0 tier 1 / $20 tier 2 / $35 tier 3 |
| Cholesterol medications | Copay: $0 tier 1 / $20 tier 2 / $35 tier 3 |
| Depression medications | Copay: $0 tier 1 / $20 tier 2 / $35 tier 3 |
| Diabetic Supplies (Including test strips, insulin pump, supplies, syringes, lancets, and more) | 0% coinsurance, deductible waived |
Source: https://mn.gov/mmb-stat/segip/diabetic-mtm-management/vbid-benefit-description.pdf
Updated January 2023 for 2023 plan year
The eligible drug list includes diabetes-specific medications such as insulin. Challenges managing one chronic condition can exacerbate an individual’s other chronic conditions. For this reason, the program also reduces prescription drug cost-sharing for members with diabetes who are also diagnosed with certain co-occurring, such as high blood pressure, high cholesterol, and depression. Drugs in tier 1, typically generic medications, are available at no out-of-pocket cost to the member, with modest copayments for drugs in tiers 2 and 3.
The list of eligible covered drugs and supplies and a series of frequently asked questions are available for members.
Unlike the Connecticut program, there is no need to enroll in Advantage Value for Diabetes. Once a plan member receives a diabetes diagnosis in the Advantage Health Plan, and the relevant claim is processed by one of SEGIP’s health plan administrators, the member automatically receives cost-sharing reductions or eliminations for all diabetes-related medical services and for all prescription drugs on the eligible covered drug list.
Future of CT and MN VBID Programs
Connecticut and Minnesota approach their VBID programs differently, but with similar goals of keeping employees, retirees, and family members healthy by incentivizing high-value care with no or low-cost access to providers and ensuring access to medications to manage chronic conditions. Given the success of their VBID programs, both states are continuing these programs, which can provide lessons for other states.