In my experience, it’s extremely hard to get heath systems to care about this stuff. It requires a level of…
Monday Morning Update 7/24/23
Top News
The Federal Trade Commission and HHS OCR send a joint letter to 130 health systems and telehealth providers, warning them that the use of online tracking technologies such as Meta Pixel and Google Analytics may create privacy and security issues that violate HIPAA, the FTC Act, or the FTC Health Breach Notification Rule.
FTC notes that companies that aren’t covered entities under HIPAA are still responsible for protecting against unauthorized disclosure of PHI, noting FTC’s recent enforcement actions against BetterHelp, GoodRx, and Premom.
HIStalk Announcements and Requests
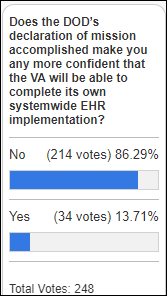
Most poll respondents don’t think that DoD’s successful completion of MHS Genesis has predictive value for the VA’s implementation of the same Oracle Health system.
New poll to your right or here: How much control should patients have in the sharing of their EHR information? I’m also interested in what providers think about receiving what seems to be a complete medical record that may have had some information intentionally hidden by the patient.
Webinars
July 26 (Wednesday) 1 ET. “Lessons We’ve Learned Since Launching our Cancer Prevention Program.” Sponsor: Volpara Health. Presenter: Albert Bonnema, MD, MPH chief medical information officer, Kettering Health System, and Chris Yuppa, product owner for oncology services and cancer prevention, Kettering Health System. Kettering’s IT department has played a critical role in providing an EHR-driven framework to bring cancer risk assessment and individual prevention plans to more than 90,000 patients. Primary care, OB/GYN, oncology, and imaging providers are now able to assess the hereditary, genetic, and lifestyle factors that affect the risk of developing lung, breast, ovarian, colon, and prostate cancer in any patient encounter. Learn how Kettering brings together people, processes, and technology to be more proactive in the fight against cancer and where its cancer prevention program is headed next.
July 27 (Thursday) noon ET. “Why You Shouldn’t Wait to Use Generative AI.” Sponsor: Orbita. Presenter: Bill Rogers, co-founder, president, and chairman, Orbita. The advent of generative AI tools truly represents a paradigm shift. And while some healthcare leaders embrace the transformation, others are hesitant. Invest 20 minutes to learn why you shouldn’t wait. When combined with natural language processing, workflow automation and conversational dialogs, generative AI can help leaders address a raft of challenges: from over-extended staff, to the rising demand for self-service tools, to delivering secure information to key stakeholders. You will learn where AI delivers the greatest value for providers and life sciences, how it can solve critical challenges faced by healthcare leaders, and how Orbita has integrated generative AI into its conversational platform so healthcare leaders can leverage its full capabilities safely and securely.
July 27 (Thursday) 2 ET. “Denial Prevention 101: How to stop denials from the start.” Sponsor: Waystar. Presenter: Crystal Ewing, director of product management, Waystar. There’s a reason denial prevention is prominent everywhere in healthcare RCM. Denials reduce cash flow, drive down revenue, and negatively impact the patient and staff experience. More than half of front-end denials don’t have to happen, but, once they do, that money is gone. It’s a pretty compelling reason to take some time now to do some preventative care on your revenue cycle. This webinar will help you optimize your front end to stop denials at the start. We’ll explore the importance of not only having the right data, but having it right where staff need it, when they need it.
Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
People

Tanya Townsend, MSMI (LCMC Health) joins Stanford Medicine Children’s Health as chief information and digital officer.
Announcements and Implementations
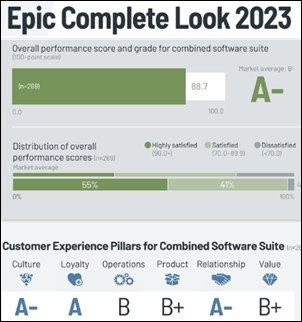
KLAS looks at the key performance grades of several EHRS and the change in their net number of hospital customers over five years:
Altera / Allscripts: D+, net loss of 143 hospitals.
Epic: A-, net gain of 434 hospitals.
Evident: D+, net loss of 91 hospitals.
Meditech: B, net gain of 14 hospitals.
Oracle Health: D+, net gain of 99 hospitals.
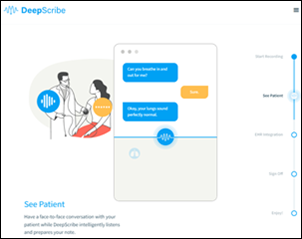
A Wall Street Journal report says that AI-powered medical scribe service DeepScribe employs a team of 200 contractors to fix mistakes made by its AI, noting that the level of inaccuracy is a reflection of AI’s limitations rather than product shortcomings. The contractors listen to the audio recordings, use Google searches to find billing codes, and catch errors. Current and former workers say the rare mistakes that slip through are always caught by the originating doctor. The co-founders say that the company’s software can create 80% of a given medical record without human help, and WSJ notes that they are transparent about that fact and the rigor of their review process in their sales presentations.
Government and Politics
ONC publishes Version 4 of the US Core Data for Interoperability (USCDI), which includes 20 new data elements and a new data class for describing the physical location of services provided.
Ashavan founder and CEO Cyrus Bahrassa urges the White House to add EHR vendor interoperability charges to its list of much-hated fees that most commonly include Ticketmaster, Airbnb, and banks. He cites the high fees associated with HL7v2 interfaces, FHIR API subscription fees, and the costs of listing and distributing apps via EHR vendor app marketplaces as “interoperability’s junk fees.”
Other
A Johns Hopkins study finds that use of hearing aids was associated with a 48% reduction in cognitive decline in high-risk people. The authors speculate that the benefit is created by a reduced need for the brain to interpret audio signals, the possible reduction in brain atrophy, and higher social activity when hearing problems are reduced.

AMA President Jesse Ehrenfeld, MD, MPH describes his view of using AI in medicine:
- The probabilistic algorithms, they’re just too narrow. They can’t substitute for the judgment, the nuance, or the thought that a clinician brings. There’s a lot of opportunity to think about these tools as a co-pilot, but not an autopilot, particularly in the diagnostic realm. That’s why the FDA’s forthcoming regulatory framework for AI-enabled devices is proposing to be much more stringent on AI tools that make a diagnosis or recommend a treatment, especially if it’s an algorithm that continues to adapt or learn over time, these so-called continuous learning systems. Algorithms are great for solving a textbook patient or a very narrow clinical question … but patients, they’re not a standardized question stem. They’re humans with thoughts, with emotions, with complex medical, social, psychiatric backgrounds. And I’ll tell you, they rarely follow the textbooks … There is an active current federal proposal that would hold physicians solely liable for the harm resulting from an algorithm if I rely on the algorithm in my clinical decision making. We don’t think that’s the right approach. We think that the liability ought to be placed with the people who are best positioned to mitigate the harm. And that is likely going to be the developer, the implementer, whoever buys these things, often not the end user, the clinician.
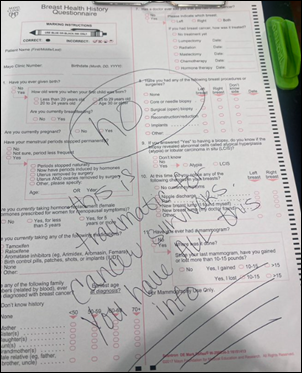
Cancer survivor and Clearsense marketing director Kate-Madonna Hindes declines to serve as the human interoperability engine for Mayo Clinic in transcribing her Epic-stored information onto a clipboard form. Twitter comments suggest that many of us are tired of being asked to restate the same information and worrying how it will be reconciled on the back end, even if few of us have her nerve to just say no (Mayo folks are always bragging on their technology expertise and commercial tie-ins, so maybe they can explain the point of such redundant analog documentation and how they process the completed form):
- “A good measure of a poorly run organization is how much of the admin work they pass on to the end user.”
- “When I had PTSD I got so sick of introducing myself & my history for half the session. Like my records are there, please take some time.”
- “I’ve started doing similar. No, I don’t need to write down each of my 20 meds on 3 tiny single spaced lines. Or my 45 years of surgical history. You have this.”
- “What it is telling me is the process is broken. Kinda like complaining to your provider about issues and at the end of the day, they want you to fill out a form.”
Sponsor Updates
- Encore Health Group and Affiliates sees success with its upgrade to EClinicalWorks V12, and Healow patient engagement solutions.
- Meditech’s Surveillance predictive analytics solution helps Golden Valley Memorial Healthcare (MO) reduce maternal complications.
- Mobile Heartbeat publishes a new e-book, “The Many Harms of Alarm Fatigue.”
- The Heidrick & Struggles Leadership Podcast features Nuance EVP and GM Diana Nole.
- Netsmart will integrate RethinkFirst’s ABA clinical solution with its suite of certified CareRecords software.
- Nordic Consulting receives 12 of 13 validations in a recent KLAS report on EHR education software and services.
- Tegria releases a new case study, “Outsourced Business Office Transforms Accounts Receivable, Increases Cash.”
Blog Posts
- Transforming Healthcare Operations Through Automation (Vyne Medical)
- 4 Ways Your Rehab Therapy Clinic May Already be Delivering Digital MSK Care (Net Health)
- Making the Case for the Collaborative Care Model at Your Organization (NeuroFlow)
- Note bloat, we can’t quit you (Nordic)
- Planning for Pharma LOE? The Digital Point-of-Care Makes a Difference (OptimizeRx)
- How to Bring Automation to Your Revenue Cycle (PMD)
- Maximize Time & Save Money Through Diverse Fax Automation Options (Vyne Medical)
- Unbelievable Stats and Other Insights from the Risk Adjustment Innovations Conference (RCxRules)
- 88% of US providers plan to increase third-party technology spending (Redox)
- Lili Brillstein’s Masterclass on How to Be Collaborative (Surescripts)
- Advance Care Planning: A Deep Dive on Advance Directives, Healthcare Proxies, Medical Powers of Attorney and Living Wills (Trualta)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



A copout by Dr Ehrenfeld – the doc should be responsible for whatever he/she uses in the clinical decision, including AI.
I think it’s a fair statement when taken in the context that the FDA has determined any “black box” AI used for clinical decision-making or treatment is a regulated device. If clinicians were solely responsible for their output they would never use those AIs because they’re incomprehensible, and we don’t exempt other manufacturers from liability in that case either.
Kudos to Kate-Madonna Hindes for pushing back against Mayo Clinic. I’m in a high risk surveillance program, and when I go for my mammograms I often get a crappy over-photocopied form to fill out. Not even a form generated out of the EHR that already has my name and DOB on it – which is totally possible with today’s technology. The last time I was there no one actually reviewed the form. It was ridiculous.
Related example of poor data handling.
I periodically have to phone my credit card company. Before connecting to an operator, they ask me to enter my CC # on the keypad. Fair enough, but when speaking to the person, they invariably ask me verbally for my CC #!
You can ask me once. You should never ask me twice, unless there is some problem on my end.
Same when calling ins companies on claims. You put the member ID in the auto attendant to even move forward in the phone system, by the time you get to a live person, all the data you previously entered needs to be spoken to the person. What’s frustrating is that many of these systems (BCBS) don’t understand the member ID’s sometimes after entering them several times both verbally and using the key pad. So much redundancy, it’s a huge time suck for billing staff doing claims follow-up.
As a parent with a medically complex child we always write ‘See Epic’ on these forms. Not once did it come up across multiple years and specialties. Always makes me wonder who’s consuming these forms, especially knowing the complex care clinic always knew exactly what was going on remotely via the chart. They could clearly make good use of the EHR.
“Re: New poll to your right or here: How much control should patients have in the sharing of their EHR information? I’m also interested in what providers think about receiving what seems to be a complete medical record that may have had some information intentionally hidden by the patient.” Who ultimately owns the patient’s health data? if it is indeed the patient, then the patient should have control of what’s disclosed, including the resulting incomplete charts being sent to another provider. The patient has the ability to choose to not tell something to a provider by simply not speaking up. Yes, omission in a chart will impact patient care, but so does omitting in person, or flat out lying. to a provider, and we all know that PaTiEnTs NeVeR dO tHaT.