Mary Madison, RN, RAC-CT, CDP
Clinical Consultant – Briggs Healthcare
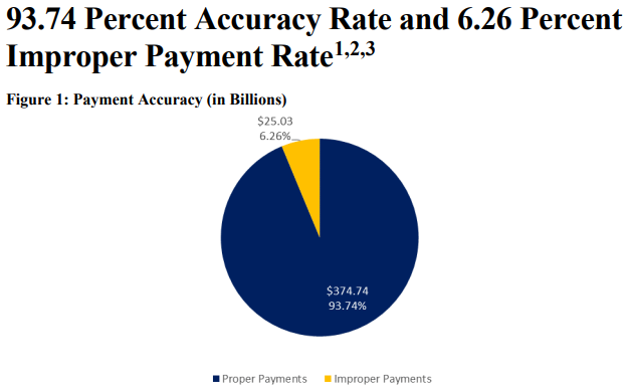
This 84-page document supplements improper payment information in the annual Department of Health & Human Services Agency Financial Report (HHS AFR). The Payment Integrity Information Act of 2019 (PIIA) requires improper payment reporting in the HHS AFR. The improper payment rate calculation complies with the requirements of Office of Management and Budget (OMB) Circular A-123, Appendix C. The Centers for Medicare & Medicaid Services (CMS) measures the Medicare Fee-for-Service (FFS) improper payment rate through the Comprehensive Error Rate Testing (CERT) program.
The report provides a great deal of information. It speaks to claims submitted July 1, 2019 – June 30, 2020 so it covers about 6 months of the initial PHE with the impact of COVID-19 addressed on page 7 of the document.
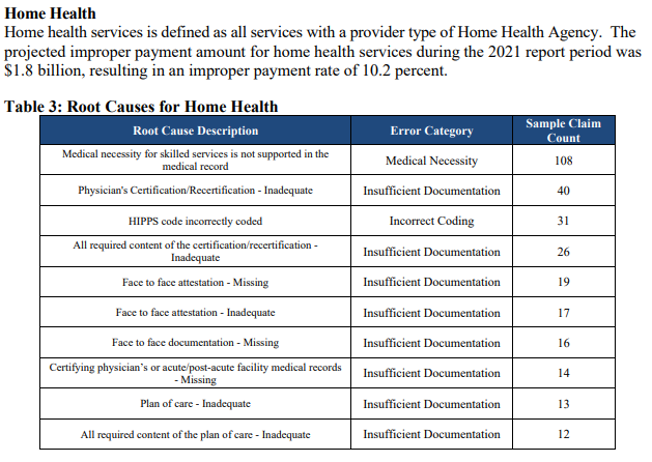
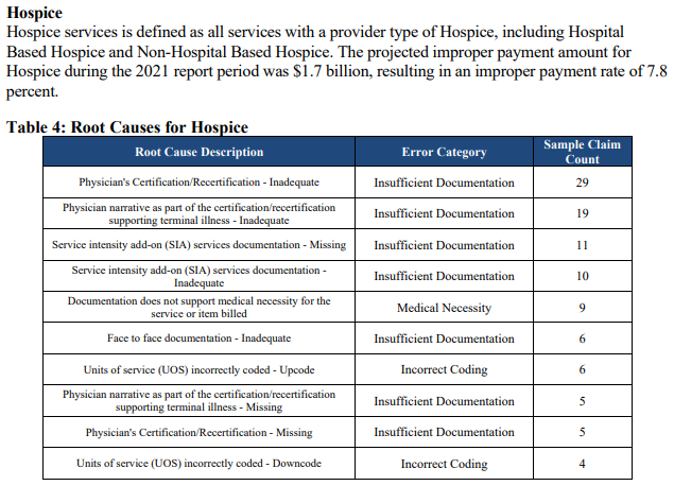
I’ve excerpted some of the charts to tweak your interest in reviewing the entire document
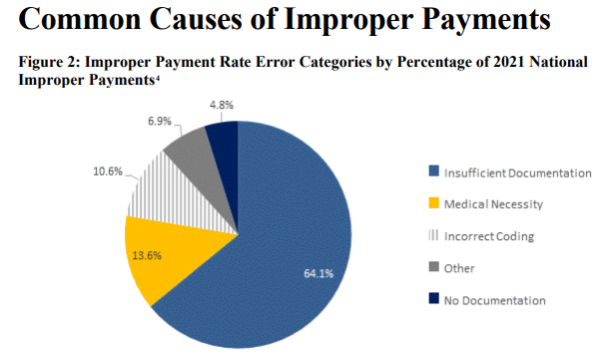
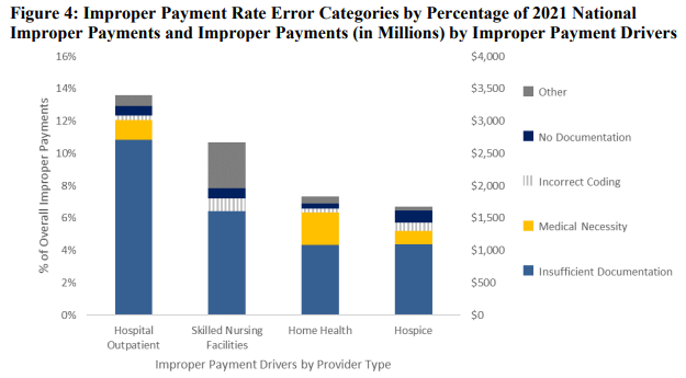
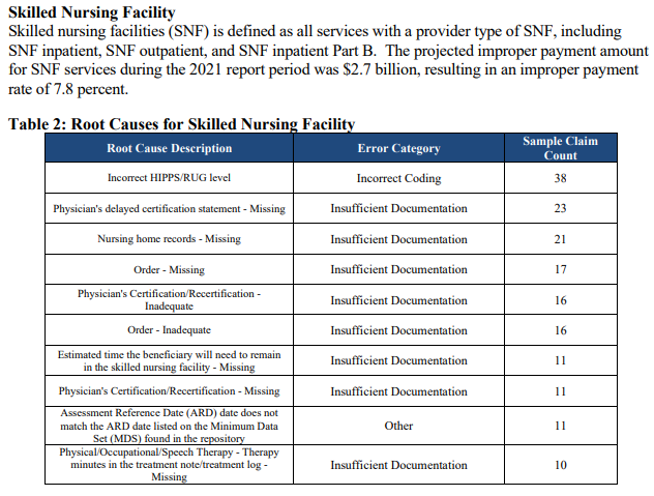
Keep reading and you’ll see information as to amounts overpaid to individual states. Beyond the initial 7 pages, the report contains lots of tables. It’s a good reminder that documentation must be accurate, complete and reflective of medical necessity.
