Mary Madison, Rn, RAC-CT, CDP
Clinical Consultant – Briggs Healthcare

Background checks for employees of long-term-care facilities are an important safety measure that can help protect some of the facilities’ most vulnerable populations. More than 13 million beneficiaries are served by long-term-care facilities each year, including the elderly, individuals in hospice care, and individuals with intellectual disabilities.
The National Background Check Program (Program), enacted by legislation in 2010, provides grants to States and territories (States) to assist them in developing and improving systems to conduct Federal and State background checks of prospective long-term-care employees. Included in this legislation is a mandate that OIG produce an evaluation of the Program within 180 days of Program completion. This report-the fifth in a series to supplement the mandated evaluation-reviews Idaho and Mississippi, the last two States that are participating in the Program. (Twenty-seven States have completed their participation in the Program.) The interim review allows for CMS to assist the States in fully implementing Program requirements during participation. In future work, we will assess the Program overall.
OIG found that Idaho and Mississippi lacked State legislative authority to implement some Program requirements. Further, both States encountered challenges with coordination between State-level departments responsible for seeking legislative authority.
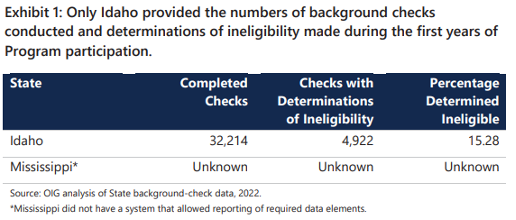
OIG found additional concerns with Mississippi. First, Mississippi was unable to submit required data to CMS to calculate determinations of ineligibility. This is despite the fact that Mississippi conducted background checks during the first years of Program participation. Additionally, Mississippi and Idaho did not consistently report Federal and State funds on required quarterly financial reports; this made it difficult for CMS to determine the ongoing cost of Program implementation.
These report findings are consistent with findings in previous OIG reports about challenges that States experienced during Program participation. Therefore, (OIG) recommends that CMS continue to implement OIG’s prior recommendations for it to take appropriate actions to (1) encourage States to obtain the necessary legislative authority from the State to fully implement Program requirements, and (2) require participating States to consistently submit data that allow CMS and each State to calculate determinations of ineligibility. In addition, with this report, we recommend that CMS ensure that participating States submit accurate quarterly reports. CMS concurred with this recommendation.
This OIG Report, released May 9, 2022, can be viewed here. It’s 31 pages in length. Below is the Table of Contents: