Mary Madison, RN, RAC-CT, CDP
Clinical Consultant – Briggs Healthcare
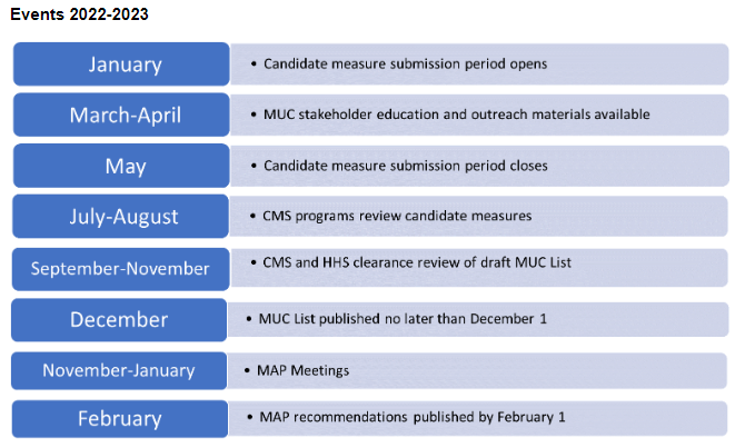
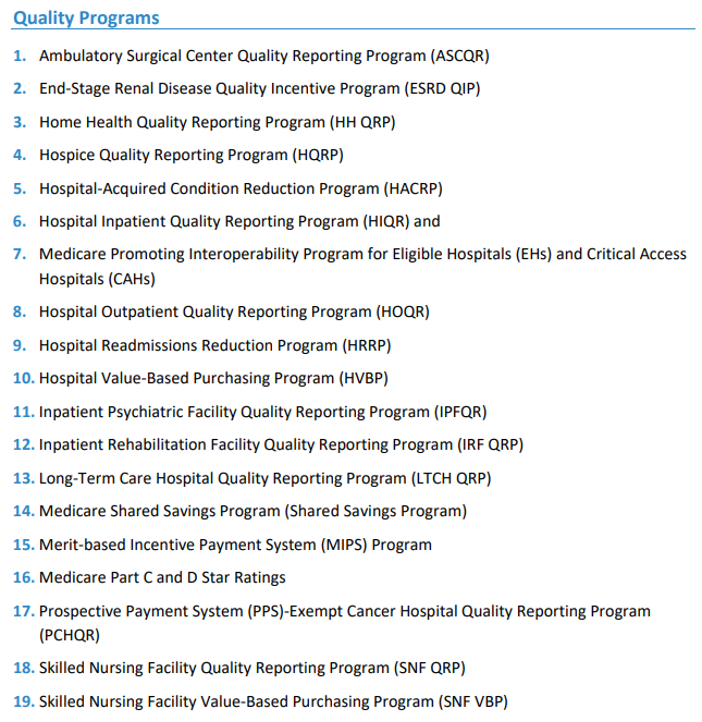
“In preparation for the statutory requirement and to remain transparent and allow for additional stakeholder feedback, each spring CMS solicits public and private stakeholders to submit candidate quality and efficiency measures for consideration by the Agency as a part of the pre-rulemaking process. The pre-rulemaking process requires that HHS make publicly available, not later than December 1 annually, a list of quality and efficiency measures HHS is considering adopting, through the federal rulemaking process, for use in the Medicare program. This list, referred to as the Measures under Consideration (MUC) List, is reviewed by a multi-stakeholder panel. The multistakeholder panel provides recommendations on behalf of the public to Department of Health and Human Services (HHS) no later than February 1 annually. For additional information on the process and information from past years, please visit the Centers for Medicare & Medicaid Services (CMS) Pre-Rulemaking website. The following programs are included in the pre-rulemaking process.
The pre-rulemaking process is mandated by section 3014 of the Patient Protection and Affordable Care Act (ACA) (P.L. 111-148, enacted on March 23, 2010), which added Section 1890A to the Social Security Act (the Act), and which requires the Department of Health and Human Services (HHS) to establish a federal pre-rulemaking process for the selection of certain categories of quality and efficiency measures for use by HHS. These measures are described in section 1890(b)(7)(B) of the Act.
Annually, CMS publishes the needs and priorities for each of the above identified programs. For each program in the pages that follow, CMS provides a brief summary of the:
• program history and structure
• current measure information (including the number of measures of each measure type)
• high priority areas for future measure consideration, and
• any program-specific measure requirements.
Through setting each program’s needs and priorities, CMS hopes stakeholders will take this into account when developing measures and submitting them to CMS for consideration on the MUC List.
CMS’s goal is to fill critical gaps in measurement that align with and support the Meaningful Measures Framework, which identifies high priority areas for quality measurement. Its purpose is to improve outcomes for patients, their families and providers while also reducing burden and moving payment toward value through focusing everyone’s efforts on the same quality areas. The Meaningful Measures Initiative also helps to identify and close important measure gap areas, align measures across the continuum of care and across payers, and spur innovation in patient-reported measures, digital measures, and new measure types.”
The 59-page Program-Specific Measure Needs and Priorities: 2022 Measures Under Consideration was posted March 30, 2022.