Readers Write: Reframing Healthcare at Home
Reframing Healthcare at Home
By Philip Parks, MD, MPH
Philip Parks, MD, MPH is partner and senior advisor at CWH Advisors of Boston, MA.
What is in store for 2024 for healthcare at home? The organizations that will be successful will make progress rethinking healthcare and reframing both the problems we are solving and how we are solving them.
Whether we think about healthcare from the perspective of a patient, caregiver, payer, healthcare provider, or technology provider, it is undeniable that three types of healthcare experiences are here to stay:
- Facility-based care. In-person care in facilities has an important place for the highest acuity clinical needs and when facility infrastructure is required;
- Virtual care. Virtual care, ranging from episodic care to primary care to mental health care, may be the best and most effective way to meet patients’ needs and wants.
- Care in the home. Virtual or in-person care (or a combination of the two) ranging from hospital home, primary care, specialty care, home health, hospice services, to in-home health evaluations for prevention and wellness.
However, the US healthcare system remains largely organized around facilities, even though the mega trends demand otherwise – aging populations with chronic conditions, adoption of technology, rising costs to support facility infrastructure, and healthcare provider staffing challenges. Therefore, many of the challenges that must be solved for moving care to the home are a work in progress. Often adoption and utilization have not been achieved to the extent needed.
While delineating care models by the site of care is practical for reimbursement and delivery of care, we are evolving to a world where patients just need care they need at the right time. The emerging concept and an example of reframing is that care can be thought of as always being on or continuous care being proactively enabled to address prevention, monitoring of treatment or care plans, navigation, and guiding the next best action for patients, caregivers, and providers.
How we accomplish this type of care in the US health system is, shall we say, a wicked hard problem that is being shaped by health and technology policies for standards information sharing (e.g., passing of TEFCA in December 2023), vertical integration (via acquisitions and/or partnerships) of providers, payers, platforms for care beyond facilities’ walls, and continued incremental innovations in care delivery models.
An often-underemphasized discipline is logistics related to healthcare in the home, especially, high acuity care in the home (or hospital-at-home) where nearly 20 types of services, supply, and staffing resources must come together on a daily basis to serve the clinical need of the patient. Factors to consider include timeliness, complexity, safety, quality, and the management and use of clinical and non-clinical data. We need more impactful partnerships between entities that bring together more integrated solutions with more value to impacting total costs of care, better use of data to directly inform evidence-based decisions and actions, and that reduce friction for patients and providers.
Five must- have tenets of a framework for healthcare services in the home should include:
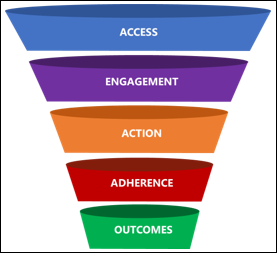
- Access. Requires making the intending action easier for patients, awareness of services, mechanism for reimbursement, efficient and cost-effective logistics, 24/7 navigation, appropriate staffing, and technology enablement support by data capture and documentation. Some examples to rethink include logistics and processes: waste disposal, reimbursement – attribution to combined service providers, technology – integration with mainstream EHRs, clinician staff that can travel, cancer care in the home, and clinically appropriate 911 diversion.
- Engagement. A mix of human touch and empathetically designed and implemented technology; very simply, engagement is the trigger for action for human behavior. Engagement must result in activation of motivation and often is a prompt of some type that is educational, motivational, or oriented toward a desired identity of being healthy. Examples of effective marketing campaigns include making the intended action by the patient or member easier by empathetically addressing “what is in it for the patient and or caregiver”. Patient and caregiver voice is critical to getting this right.
- Actions. These are the evidence-based behaviors by the provider and the behaviors of the patient (and caregiver) to participate in self-care or provided care. An example of options for home care is direct to consumer campaigns for colorectal cancer screening, which provide information based on the member or patient’s preferences and risk for colorectal cancer and in some cases can be done at home.
- Adherence. Repeated behaviors related to self-care and active participation in provided care. Critical for adherence are literacy, knowledge, motivation, and ability. Making the repeated action as easy and simple as possible is critical. Examples of effective adherence strategies at home include enlisting the caregiver to reinforce self-care, using technology enabled reminders to prompt good habits, and ensuring that resupply of medications and supplies are automated when possible and medically necessary.
- Health outcomes are a function of proactively creating access to all people and populations, proactively engaging with education and motivation that must lead to action on the part of patients. Adherence or repeatable actions result in outcomes.
Care at home may be the best site to conduct early screenings and pick up on other factors that wouldn’t necessarily happen in traditional settings. Also, with some diseases, the time period of screening and early detection may be much faster when screening can occur at home. For example, for individuals at average risk for colorectal cancer, samples can be collected in the home and mailed in for evaluation.
These tenets are the most important attributes which must be part of patient-centered design of services in the home. Obsessing over the healthcare and lived experiences of patients, caregivers, and their healthcare provider team members is paramount.
Reframing healthcare at home offers immense potential benefits related to quality of care, decreased costs and improved outcomes, elimination of silos across the continuum of care, and high satisfaction for patients, caregivers, and providers. Perhaps one of the most actionable ways for determinants of health to be identified and addressed is through continuous engagement and support to patients via care navigation, coordination, and the provision of clinical and non-clinical services in the home.


What are the forthcoming minimum cybersecurity standards?