Readers Write: Accelerating Redetermination: Social Drivers of Health and 1115 Waivers
Accelerating Redetermination: Social Drivers of Health and 1115 Waivers
By Jaffer Traish
Jaffer Traish is COO of Findhelp of Austin, TX.

Medicaid Redetermination
Medicaid continues to be the largest healthcare funding vehicle in the United States. From February 2020 to April 2023, Medicaid and the Children’s Health Insurance Plan (CHIP) enrollees increased 33% to 94 million individuals.
The declaration of the public health emergency (PHE) by Congress in March 2020 enacted a “continuous coverage” requirement, where Medicaid agencies couldn’t disenroll anyone unless they asked, moved out of state, or passed away. Traditionally, there is a churn or loss of enrollees due to non-responsiveness to forms requests, regular eligibility reviews, income changes, and so forth. When the PHE ended on May 11, 2023, state Medicaid agencies were given 12 months to initiate renewals and 14 months to complete them. For many states, unwinding from the PHE will last well into 2024.
Redetermination processing is an enormous undertaking. States are under pressure from the Centers for Medicare and Medicaid Services (CMS) which can track call center metrics and procedural terminations (for example, if the person couldn’t be reached). CMS could even request corrective action plans and implement financial penalties in the event of missed unwinding reporting as required by the Consolidated Appropriations Act.
Being a Medicaid director is a critical yet unenviable position for PHE unwinding, and some states have requested waivers to use simplified criteria to process redeterminations. It has been estimated by Kaiser Family Foundation that a staggering eight to 24 million enrollees may lose Medicaid coverage.
Innovating with CMS Waivers
One approach available to states, and growing in popularity, is the 1115 Waiver. The Secretary of Health and Human Services (HHS) can approve a waiver for a pilot or demonstration project that federal rules would normally not allow, including changes to eligibility, benefits, and provider payments.
As of August 2023, there are 68 approved 1115 waivers across 48 states. Interestingly, 19 of these have social drivers of health provisions. There are 33 more waivers pending approval, and 12 of these also include social drivers of health provisions.
Beneficiary Stability
By investing in non-traditional case management, housing, and nutrition, states are adding stability for enrollees with specific health-related social needs and anticipate a positive impact on redetermination. New York, for example, is awaiting approval on a several billion dollar waiver proposal to invest in creating major social care network structures.
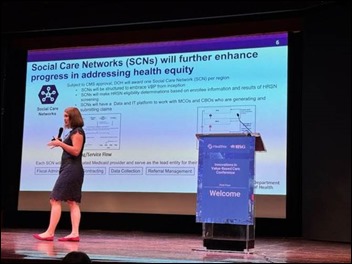
Amanda Lothrop, COO of Medicaid for New York State, shared the significant role social care networks will play in the 3.5 year demonstration waiver to a large group of NY stakeholders on September 27.
Centene, UnitedHealth Group, Elevance Health, Molina, and Aetna control about half of the Medicaid Managed Care market across 40 states. They receive requests from states for both updated enrollee contact information to better process redetermination and to meet requirements for social care provider networks and claim processing as part of their benefit administration.
Three Themes: Understanding the Evolving Medicaid Population
In discussing these challenges with managed care organizations, government, schools, hospital systems, and community organizations, we hear three consistent themes:
- States are in the dark about the non-medical risks of enrollees and how this is impacting churn and cost. In particular, MCOs need early notification about the clinical and social risks of both adults and children. Not only to work to address them, but to conduct benefit eligibility determinations and proactive engagement.
- Hospital systems need to adapt to new Medicaid-led financial incentives to assess needs and initiate interventions. States may take for granted the community engagement (trust-building), network contracting, and technology implementation that is required for successful non-medical services delivery.
- A single care coordination technology mandate does not substitute for community interoperability. Care coordination is cross-sector and collaboration goes far beyond traditional healthcare. All industries should look to United States Core Data for Interoperability (USCDI) standards and follow rules such as the Michigan Health Information Network (MiHIN) interoperability pledge.
The Future of Redetermination
To stay rooted in reality, waivers come and go, as do the officials that approve them. In the long term, states should invest in enhancing their member engagement channels to reduce procedural termination, updating their public health analytics to include social risk, and reducing paper friction in the state benefit eligibility processing.
The Kaiser Family Foundation estimates that more than 4 million people have lost Medicaid coverage so far. States do not have to make redetermination data public, so the full scope is unknown until federal numbers are published later this year.
Imagine if:
- The MCO could retrieve current member contact information and social risk through hospital electronic health record (EHR) connectivity to contact members for redetermination and support. Epic Payer Platform and SchoolCare are two examples of vendors supporting these efforts.
- The acute and post-acute care providers could order waiver-approved social services based on automatic benefit authorization. CalAIM is an example of this enhanced care management.
- The community social service provider could document services and reimbursement codes would automatically associate in the system for claims. MassHealth supports codified services in this approach.
- States aggregate anonymized social risk, supply, and demand to inform future capacity investments and waiver services to expand or retract. CRISP HIE in Washington, DC is leading efforts in aggregated social services management.
The large redetermination effort nationwide and the requests by states to fund social services for beneficiary stability are fueling a renewed look at antiquated state benefit eligibility systems and processing. One prediction – we will start seeing API-based application submissions that enable fast determination and financial disbursements for state benefits.
We will be watching (and supporting) waiver implementations closely along with private sector investments in social drivers of health to better understand public benefit needs, direct service delivery, and accelerated redetermination.


Pen and paper is not the downtime system a health system should be using in 2024. A local non internet…