EPtalk by Dr. Jayne 1/25/24
I had dinner the other night with a group of family physicians. It was an interesting bunch. Three of them have left employed practice models to open their own primary care practices. One is practicing with the local visiting nurse association. Another is working as the medical director for a local hospice. Several are on faculty at residency training programs, and two of us are clinical informaticists.
As one can imagine, telehealth was a hot topic. One of the physicians who is employed by a local health system was complaining about how her organization has brought in a third-party vendor to perform urgent care telehealth visits. In particular, she feels that continuity of care has suffered. One of our colleagues mentioned a recent study that was published in JAMA Network Open that looked specifically at virtual visits that were performed by the patient’s own family physician compared to those that were performed by an outside family physician.
The authors looked at 5 million Ontario residents who met criteria for having a family physician and for having had a virtual visit. They concluded that visits with an outside physician were 66% more likely to be associated with an emergency department visit in the next seven days compared to those visits that were conducted by the patient’s own physician.
If you dig deeper into the results, they looked at a matched subset of patients and found that the changes of an emergency department visit in the next week was even greater for patients with “definite direct-to-consumer telemedicine visits.” They specifically excluded virtual visits that were performed by another physician in the same group as the family physician, since they “sought to contrast the highest-continuity virtual visits (own physician) with lowest-continuity virtual visits (outside of group).” The authors go on to conclude that the findings “suggest that primary care virtual visits may be best used within an existing clinical relationship.”
The authors noted that increased emergency department utilization that were associated with low-continuity visits suggest that “virtual visits may serve a triaging function, allowing for the identification of patients who would benefit from an in-person assessment.” It would be interesting to see a similar study performed in the US, since there are likely differences in service utilization due to the payment landscape here. When patients are worried about co-pays and emergency department costs, they often make different decisions than they might if they were part of a system where they were at less exposure for unexpected healthcare bills. The authors noted that one of the limitations of the study was the lack of ability to identify patients where access was an issue, such as hours of clinic operation, physician availability, or scheduling difficulties.
The next time I see them, I’ll have to get my family medicine colleagues to weigh in on “The Case of the Disappearing Thank Yous,” which was published in JAMA Health Forum earlier this month. It begins by detailing a physician’s dissatisfaction when her employer began to filter messages from patients that said, “Thank you.” Although some may feel that such messages represent clutter, including EHR vendors who have acted on client requests to suppress them, this physician found them meaningful.
It’s the classic case of whether the good of the one outweighs the good of the many, but the author went on to discuss other ways that he feels that appreciation of accomplishments is lacking in healthcare. As an example, he mentions that Medicare costs have stabilized and that important public health worth continues to progress despite the persistence of negative headlines.
He mentions what most of us already know – negative news tends to generate more clicks than positive news. It’s all about monetizing those eyeballs. He notes that “a failure to appreciate past victories can also jeopardize efforts to tackle the health challenges of the future,” especially in the setting of low trust for government agencies which includes those that are involved in public health.
Especially for healthcare workers who have really taken a beating over the last several years, it’s important to feel appreciated. Employers tried to say thank you by issuing challenge coins and sending pizza, but it’s time to figure out how to demonstrate appreciation in a meaningful way. I know I would like to grow old in a society with highly qualified nurses that love their jobs, but the chances of that being a reality are becoming smaller every day. Here’s a challenge to administrators to start figuring out what really matters and putting their money to work.
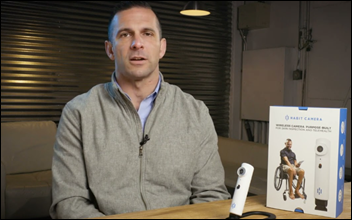
I’m always on the lookout for healthcare technology that has an interesting backstory. Habit Camera is a wireless camera that is designed to allow users to inspect areas of the skin that they might not otherwise be able to see. Daily skin inspection is important for many patients, including those with diabetes, limited sensation, or active wounds. The camera connects to a smartphone app to enable live viewing of high definition images as well as video and image capture for sharing with clinicians or caregivers. The company is led by a US Marine Corps veteran who was paralyzed while serving in Afghanistan. He and his wife run the company, which employs veterans and their family members to assemble the devices.
I particularly liked the answer to one of their FAQ questions, which asks, “Is my clinician going to look at pictures if I send them?” The response: “It depends! Your clinician may be interested in doing this, but some may not. If you can’t share an image or video with your clinicians, then it can be really hard to explain what you see over the phone. Until a clinician can see it with their own eyes, they probably will ask you to make an appointment and come into clinic. This can be a bit of a hassle, especially if you have to take off of work and drive far, so we hope that pictures and video can help reduce unnecessary visits. A picture is worth a thousand words.” I don’t care how much a company pays for its marketing experts; you really can’t portray the patient experience any better than that.
What technology vendors have the best messaging? Is there a particular one that you feel just tells it like it is? Leave a comment or email me.

Email Dr. Jayne.


I agree. My experience has been that failure conditions vary quite a lot. This causes tremendous variations in how the…