The Blue Cross Blue Shield Association (BCBSA) hopes to bolster its campaign for site-neutral payment reform with the release today of an issue brief (PDF) that enumerates how much more certain routine healthcare services for commercially insured members cost in hospital outpatient departments than they do in physicians' offices or ambulatory surgery centers.
“Our analysis of national Blue Cross Blue Shield data found that allowed costs for common outpatient services were consistently higher in the HOPD setting than for those rendered in an ASC or office location,” according to the issue brief. “For all of the examined procedures except clinic visits, allowed costs also grew faster in the HOPD setting.”
David Merritt, BCBSA’s senior vice president of policy and advocacy, said in a statement that “lowering the cost of care, regardless of the site, is common sense. Our analysis shows site-neutral legislation could save our patients, businesses and taxpayers nearly $500 billion over 10 years. We look forward to continuing our work with Congress to protect patients from these higher costs.”
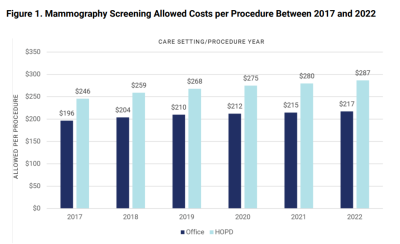
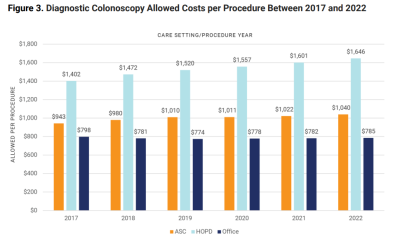
BCBSA researchers analyzed PPO commercial claims data for about 133 million members from 2017 to 2022 (for office visits, the time range was 2014 to 2022). They looked at six procedures: cataract surgery, chest X-ray, clinic visits, colonoscopy (diagnostic and screening), ear tympanostomy and mammography.
Allowed costs for all the procedures except clinic visits also grew faster over the six years at HOPDs than they did at physicians' offices and ASCs. For example, mammograms cost 32% more in an hospital outpatient setting than in a doctor’s office. Diagnostic colonoscopies cost 58% more in an HOPD than in an ASC.
“In conclusion, our findings suggest that if commercial payers implemented site-neutral payments across settings, then employers, employees, and patients would realize substantial savings through lower premiums and out-of-pocket costs,” the issue brief states.
As to exactly why this happened, researchers admitted that they were stumped, although they cited several possible reasons. “These include market forces resulting from physician and hospital consolidation, hospitals passing on the higher costs of delivering care regardless of settings, the financial impact of COVID-19 on providers and insurers, and variation in severity of illness across settings. Future studies will address the root cause of these pricing differences and other questions.”
Some of those future studies will be done by the American Hospital Association (AHA), which worries that BCBSA wants to take site-neutral payment reform in the wrong direction. AHA argued that hospitals treat sicker and more complex patients and have more of an overhead.
A report done by KNG Health Consulting for the AHA and released in April reviewed Medicare claims and found that HOPDs treated a greater number of individuals with severe comorbidities. In addition, this group more often used the emergency department or has a short-term admission within 90 days of an outpatient visit.
The AHA report stated that “patients of higher complexity may require a greater level of care than patients of lower complexity. To the extent that these differences result in variations in the cost of care, site-neutral payments may have adverse effects on patient access to care.”
BCBSA circles back to the consolidation of physician practices and hospital systems over the last two decades that resulted in 52% of physicians being employed by hospitals or health systems. This gives providers much more clout when they sit down to hammer out a new contract with health plans, according to the issue brief.
HOPDs bill for two types of service: the physician fee and the fee for using the facility.
“HOPD facility fees are meant to cover the higher costs associated with running a full-service hospital and are significantly higher than the reimbursement for the technical components associated with free-standing physician offices or ASCs,” according to the issue brief. “Commercial health insurance payment policies are determined in contract negotiations between the health plan and the provider. However, it is also quite common for health plans to pay a much higher rate (including the facility fee) for procedures delivered in HOPDs.”