Community health workers (CHWs) have played a key role in states’ COVID-19 responses, and federal funding opportunities have expanded the CHW workforce through an infusion of time-limited funds. As states are seeking sustainable financing models and partnerships that offer continued support for the CHW services beyond the COVID-19 pandemic, many are exploring Medicaid reimbursement models.
Existing approaches include submitting Medicaid state plan amendments (SPAs) or seeking 1115 demonstration waiver authority to reimburse CHW services. A few states are exploring alternative payment models (APMs). APMs can provide an alternative to Medicaid fee-for-service reimbursement that may help incentivize inclusion of CHWs on care teams and better anticipate the types of services CHWs offer. Additional detail about state-specific approaches can be found via NASHP’s 50-state scan or a recent issue brief detailing state approaches to authorizing CHW reimbursement using SPAs.
NASHP regularly convenes state health officials to discuss policy strategies related to financing and infrastructure for the CHW workforce. During a recent virtual meeting focused on alternative payment approaches, Maine state officials detailed how the state intends to use its Primary Care Plus (PCPlus) program to reimburse for CHW services.
What is Maine’s PCPlus program and how does it support CHW services?
What is an Alternative Payment Model?
According to the Centers for Medicare and Medicaid Services (CMS), “an Alternative Payment Model (APM) is a payment approach that gives added incentive payments to provide high-quality and cost-efficient care. APMs can apply to a specific clinical condition, a care episode, or a population.”
CHWs have been long established in Maine. With their critical role in the state’s COVID-19 response, there has been increased recognition of how CHWs can help to improve community health. In July 2022, Maine launched the first phase of its new PCPlus initiative, which is an APM through MaineCare, Maine’s Medicaid program, that provides a higher per member per month (PMPM) rate for a whole-person care approach that includes services such as care coordination, health and oral screenings, and care transition.
The goal of the PCPlus initiative is to provide primary care practices with more flexibility in care delivery while reducing inefficiencies. With CMS approval, more advanced elements of the initiative will provide incentives to primary care practices that offer CHW services.
How is the PCPlus program structured?
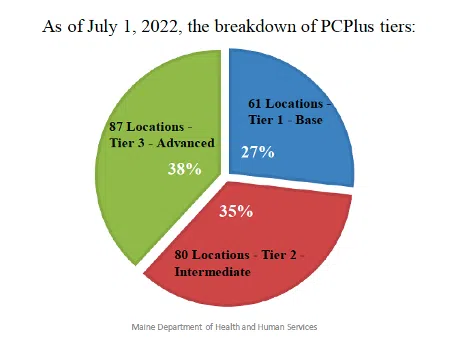
The PCPlus program is structured on three tiers of service requirements, with the potential reimbursement rate increasing with each tier.
Tier 1 includes basic requirements such as using a certified electronic health record. To meet advanced tier requirements, practices must meet the standards of the previous tier (e.g., to be eligible for Tier 2 reimbursement rate, a practice must meet Tier 1 and Tier 2 requirements).
In addition to requirements such as the provision of medication for addiction treatment services, telehealth, care coordination, and monitoring social needs, Tiers 2 and 3, once approved by CMS, would require primary care practices to provide CHW services by either hiring CHWs or contracting with CHW organizations.
The program will provide technical assistance to practices interested in meeting service requirements necessary to advance through the tiers. As of July 1, 2022, practices meeting Tier 2 and Tier 3 requirements make up 73 percent of all participating PCPlus practices (see image below).
PCPlus introduces CHW services using a phased approach. Providers must produce an environmental scan identifying how populations served by primary care practices may benefit from CHW services. Including a scan also helps the state assess practices’ needs and take their varying knowledge of CHW roles into account. The state intends to use this information to support CHW work across the state as well as identify technical assistance opportunities for practices. After the scan is complete, practices would be able to develop a plan for providing CHW services either directly (by hiring CHWs) or through partnerships and contracts (e.g., with community-based organizations or CHW organizations).
Beyond payment, how is Maine approaching sustainable infrastructure for the CHW workforce?
In addition to the PCPlus program, the state is developing other ways to engage with CHWs and build infrastructure that bolsters the workforce.
The Maine CHW Initiative (MECHWI), the state’s CHW network that was developed through a collaboration between the Maine CDC and partners after the conclusion of the Maine State Innovation Model project, has created an advisory committee to help guide the network through developing a strategic plan. Half of the members of this group identify as CHWs. Drawing from this model, MaineCare is working with MECHWI to convene a CHW advisory group to guide the development of health care delivery and payment models involving CHWs within PCPlus.
What are other states doing related to CHW services and APMs?
The Blueprint for Health is in Vermont state statute and uses multi-payer model (Medicaid/Medicare and commercial payers) to support patient-centered medical homes through funding, training, and support. These funds are distributed to administrative entities and allow the community to hire a variety of staff based on needs identified through community health needs assessments and other community partnerships. The community may choose to hire CHWs to support these goals.
Vermont is currently in the beginning process of identifying additional sustainable funding models that can support CHWs in a variety of settings. The Vermont Department of Health and the CHW Steering Committee are leading this work.
Authorized by SB 184, California will be implementing an APM with a subset of its federally qualified health centers (FQHCs) starting in 2024. Currently, both managed care plans and FQHCs pay for CHW services. CHWs play a critical role in implementation of the California’s Advancing and Innovating Medi-Cal initiative, a statewide effort to strengthen the state’s Medicaid program by offering Californians a more equitable, coordinated, culturally competent, and person-centered health care services. The APM will provide FQHCs with greater flexibility in care delivery approaches that meet this objective by moving away from a volume-based reimbursement.
North Carolina plans to incorporate CHWs as “care management extenders” within the state’s Medicaid managed care prepaid health plan care management models. Care management extender roles will fit into the existing PMPM capitation payment model.
In addition to existing “Standard Plans,” the state will launch “Tailored Plans” on April 1, 2023. These plans will offer integrated services to enrollees with significant behavioral health needs and intellectual/developmental disabilities.
Care management extenders can support care managers and help meet member contact requirements. CHWs who have completed the North Carolina CHW Standardized Core Competency Training will meet the extender qualification requirements.
The state is also exploring an additional PMPM capitation payment structure via its contract authority with Standard Plans that would establish a CHW staffing requirement ratio. The goal of this ratio would be to expand the number of CHWs deployed throughout its Medicaid managed care system. The state is also considering how health plan-level requirements filter down to providers with local care management responsibilities and how to encourage community-based organization partnership and deployment of CHWs. Current guidance was provided in July 2022. Additional guidance is expected in July 2023.
NASHP will continue to track these approaches as they emerge and develop.
Acknowledgments
NASHP would like to thank state officials from Maine, Vermont, North Carolina, and California for providing information for this blog.
Support for this work was provided by the Robert Wood Johnson Foundation. The views expressed here do not necessarily reflect the views of the foundation.




