Why You Should Share Behavioral Health Notes With Patients
You might feel a little nervous when you think about writing behavioral health notes your clients will read. You know some of your clients may experience distress viewing their progress notes, while others could certainly benefit from the increased transparency. Although some exceptions exist, in general, sharing your clinical documentation can boost client engagement and give them greater control of their mental health. Depending on your practice, you may be legally required to share your notes.
New federal rules under the 21st Century Cures Act (Cures Act) will require all health care providers or "actors" to give patients access to their records in an electronic health record (EHR) system. This includes community mental health centers, clinical social workers, clinical psychologists and psychiatric hospitals.
Even if the legislation does not apply to your practice, you may still consider sharing your notes with clients due to its advantages. This post will show the benefits and challenges of sharing your therapy notes and provide tips for creating documentation you feel comfortable viewing with your clients.
Table of Contents
- Are Therapy Notes Confidential?
- Do Therapists Share Notes?
- Should Therapists Share Notes?
- Benefits of Sharing Therapy Notes With Patients
- 6 Tips for Writing Shareable Therapy Notes
- Preparing for Challenging Situations
- How to Balance Risk and Respect When Sharing Therapy Notes With Patients
- Request Your Free Trial of ICANotes
Are Behavioral Health Notes Confidential?
Under the Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule, clients do not have a right to access their therapist's or psychologist's psychotherapy notes. Psychotherapy notes are a counselor's private notes, and they do not include information maintained in clients' medical records — such as medication prescriptions or treatment plans.
The primary purpose of psychotherapy notes is to help behavioral health professionals do their job better. Although psychotherapy notes can be kept confidential, counselors generally have a right to share them if clients ask to see them.
When the new information blocking rules go into effect in April 2021, psychotherapy notes are exempt, but only if they are maintained separately from the client's medical record. In addition, the April 5 ruling does require the sharing of medication prescription and monitoring, counseling session start and stop times, the modalities and frequencies of treatment furnished, results of clinical tests, and any summary of the following items: Diagnosis, functional status, the treatment plan, symptoms, prognosis, and progress to date.
Under the Cures Act, healthcare providers will be required to share the following types of clinical notes with patients as outlined in the United States Core Data for Interoperability:
- Assessments
- Diagnoses
- Treatment plans
- Progress notes
- Laboratory reports
- Medical histories
- Discharge summaries
Clients already have a right to request their medical records under HIPAA. The Cures Act will make it easier for patients to access their information online through patient portals.
Do Therapists Share Notes?
According to OpenNotes, an international movement dedicated to increasing health care transparency, a growing number of healthcare professionals are sharing behavioral health notes with clients. For example, social workers, psychologists and psychiatrists at Beth Israel Deaconess Medical Center in Boston began sharing notes with nearly a thousand patients shortly after doctors published an article suggesting the value of open notes in 2014.
OpenNotes states that in 2020, over 250 health organizations across the United States have chosen to offer open notes to more than 50 million patients through patient portals. While many private practice therapists may not yet provide clients easy access to their notes, there are plenty of reasons to consider the options.
Should Therapists Share Notes?
Many therapists are uncomfortable sharing notes with their clients. As mentioned in an article published in the AMA Journal of Ethics, mental health professionals may be reluctant to share notes due to the ethical principle of nonmaleficence — which means to do no harm. Reading behavioral health notes could cause clients anxiety or confusion, and some might be offended by what they read.
Knowing the risks, counselors need to consider how clients might react as they create notes. Behavioral health professionals also need to think about each patient's condition before inviting them to read their notes. In some cases, healthcare providers aren't required to share their notes. The Cures Act includes the following exceptions:
- To substantially reduce the risk of harm
- To protect the individual's privacy
- To protect the security of electronic health information
- If it's not feasible due to an uncontrollable event, such as a natural disaster
- To temporarily perform maintenance on health information technology
With that said, reading behavioral health notes has many positive effects on patients, and it's what they want. According to a survey published in 2019 that examined patients' views on reading their behavioral health notes online, 94% said they think it's a good idea to have open notes, and 87% want it to continue.
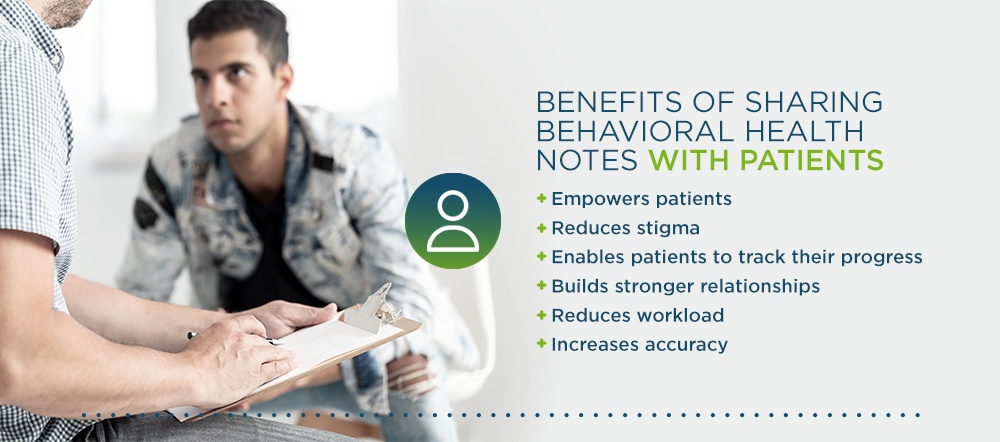
Benefits of Sharing Behavioral Health Notes With Patients
Some patients may choose not to read their behavioral health notes. Those who do may become more engaged with their health care and more trusting of their doctors. Overall, sharing your notes offers several advantages for your clients and your practice:
- Empowers patients: Note-sharing promotes collaboration and communication between patients and providers. Collaborative decision-making shows patients they are capable of discussing their notes and taking control of their health.
- Reduces stigma: Note-sharing removes the mystery from therapy and decreases the stigma attached to mental illness. When clients read notes written by behavioral health professionals, they can feel more understood, less afraid of stigma and more willing to address mental health issues.
- Enables patients to track their progress: When clients read their progress notes, they can identify areas in their treatment plan that work and those that need adjustments. As a result, clients can work with their therapists to fine-tune their treatment plans and increase the effectiveness of their therapy.
- Builds stronger relationships: Sharing notes with clients helps them develop a stronger sense of trust in their healthcare providers and improves relationships. For example, in surveys following up with patients after reading their clinicians' progress notes, 37% reported feeling better about their doctor. The providers themselves reported perceiving greater patient trust and satisfaction.
- Reduces workload: When patients read their notes, they can review what happened in their last session and better prepare for their next appointment. Clients may even contribute to their notes in their clinician's EHR. For example, the OurNotes philosophy encourages patients to briefly describe how things went between visits in the patient portal. Their notes help create more focused visits and remove some of the workloads for clinicians.
- Increases accuracy: Documentation errors are common. According to a recent survey that examined errors in ambulatory care notes, 1 in 5 patients who read their notes found a mistake, and 40% felt the error was serious. By sharing your notes with clients, you allow them to review critical information about their medications and medical history and give them a chance to point out inaccuracies.
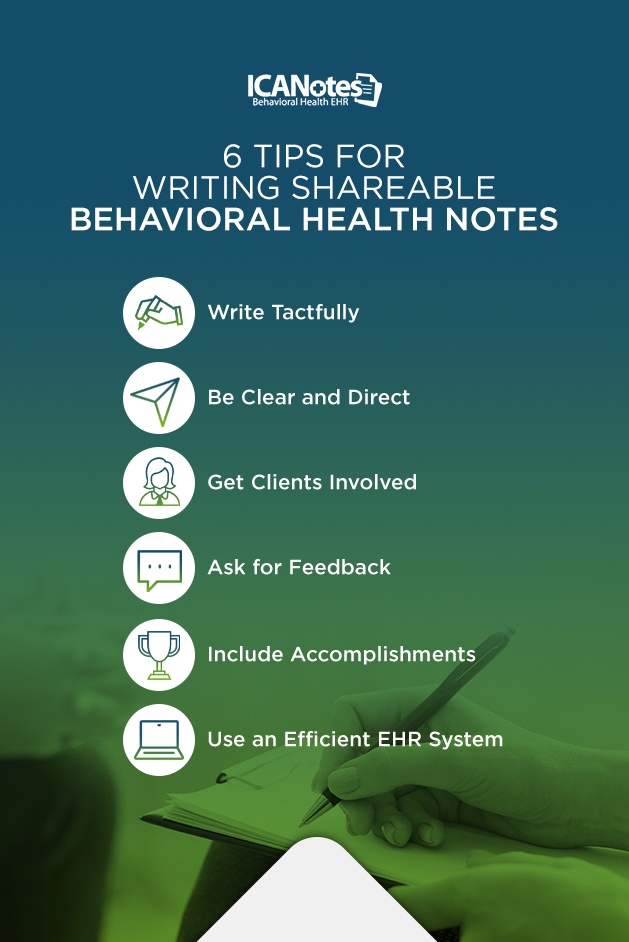
6 Tips for Writing Shareable Behavioral Health Notes
Clinicians may be concerned about sharing notes covering sensitive topics, such as abuse or substance use disorder. While it's true that challenges exist, there are ways to create notes that address difficult topics with clarity and sensitivity. You'll always want to assume clients will read your notes, even if they don't express interest in doing so.
Here are tips for writing shareable behavioral health notes that will help clients understand their diagnosis and feel supported:
1. Write Tactfully
Choose words carefully when covering sensitive topics to keep clients from feeling offended. For example, rather than writing that a client "refuses" treatment for alcohol use, you might instead say the client "chooses not to pursue" treatment. Another way to use nonjudgmental language is to include information as quotes said by the patient, rather than put details in your own words. For instance, rather than writing that a patient drinks heavily, you might write, "The patient states, 'I drink every day but can stop when I want to.'"
It's essential to avoid the use of stigmatizing language in your notes. For example, rather than describing a client as an addict, write that they have a substance use disorder. As a general rule, write only things you'd feel comfortable saying in front of the client. It's also a good practice to only write about the topics you discussed with your client.
2. Be Clear and Direct
Clients should be able to understand your notes. Avoid using abbreviations, acronyms and medical jargon, and aim to write clear and concise notes. By using straightforward, simple language, you'll increase readability and decrease documentation time. An article published in The American Journal of Medicine provides the following tips for writing helpful notes:
- Use a bold font for instructions and other important details.
- Consider writing in the second person, using the pronoun "you."
- Add links to online educational resources to clarify medical terms.
If you need to include certain details for insurance purposes, make sure you explain to clients what you write and why. Transparency is key to building trusting relationships.
3. Get Clients Involved
It helps to get clients involved in the note-taking process and discuss what you'll write in your notes. You might even turn your computer screen toward your clients so they can watch you as you write and give their input. Make sure clients understand you have to meet specific professional requirements as you take notes.
You may also want to talk to your clients about any details they wish to omit from their clinical notes. Let them know you value their privacy, but you also want to ensure continuity of care, and you may need to prove the medical necessity of their treatment. Work with them to find the right balance between protecting their privacy wishes and providing the best care possible. The point of engaging your clients is to encourage open communication and eliminate confusion.
4. Ask for Feedback
Encourage clients to check the accuracy of your notes and provide feedback. Let them know you'll be happy to resolve any issues during their next visit. Also, remind each client that you're working together as a team to help them reach their goals and that their feedback makes a difference.
5. Include Accomplishments
Make sure your notes do not only focus on a client's issues. Be sure to include their accomplishments and progress as well, so you can encourage them to stay on track. For example, instead of writing that a client still needs to lose 20 pounds, you might write that they lost 5 pounds and are motivated to reach their goal.
6. Use an Efficient EHR System
It's essential to consider your EHR system and how you'll create and share your therapy notes with clients. Ensure you choose an EHR that facilitates simple and accurate note-taking and provides a secure, easy-to-use patient portal that clients can access to read their records. By selecting an efficient EHR system, you can help prevent technical issues, speed up documentation time and enjoy streamlined communication with clients.
Preparing for Challenging Situations
While there are many advantages to sharing behavioral health notes with patients, it can potentially lead to challenging situations. Here are a few examples of issues you might face resulting from note-sharing and ways to handle them:
1. The Client Disagrees With You
There may be times when a client disagrees with your notes and your professional judgment. If tension arises between you and a client due to a disagreement, include their thoughts in your notes. For example, if a client believes you misdiagnosed them, you might add to your notes that the client disagrees with your diagnosis. Let the client know you cannot change your medical judgment, and encourage an open discussion to address their concerns.
2. There's Potential for Harm
In some cases, offering easy access to a client's behavioral health notes could be harmful. For example, you may need to consider if a client lives with an abusive spouse who might read their notes.
Make sure patients understand your practice's mental health records release policy and ask them if they have any concerns. If they fear a household member will access their notes, you might not use your EHR to exchange information. Instead, consider discussing your notes with the client privately during therapy sessions.
3. The Client Does Not Want to Include Traumatic Experiences
If a client does not feel comfortable documenting the details of a traumatic experience, you have other options. Rather than describe the trauma in your notes, you might write that the client mentioned a significant incident from their past and that you will continue to explore the incident in your next visit.
How to Balance Risk and Respect When Sharing Behavioral Health Notes With Patients
Writing shareable notes involves finding the right balance between risk and respect. You don't want to offend your clients, but at the same time, you need to include accurate, truthful information that will help them get the proper treatment.
Keep in mind that you need to consider your client's wishes when creating notes. As the American Psychological Association states, there are no laws that require you to include sensitive details. You'll need to use your judgment when you write and consider if certain details are necessary. You might include information in your private psychotherapy notes instead of your clinical documentation to help you provide care.
Also, don't be afraid to reach out to colleagues for guidance before you implement open notes. Learn ways to write empathetic and clear notes that will keep your clients engaged. Be prepared to advise your clients on reading your notes and encourage them to share their concerns with you.
Request Your Free Trial of ICANotes
Sharing your notes may be a completely new experience for you and your clients. The first step to note-sharing is to set up a reliable, secure and intuitive EHR system. Your EHR will give your clients access to their information through a patient portal. At ICANotes, we're ready to help you get started.
ICANotes is EHR software designed for behavioral health professionals. With ICANotes, you can quickly create legible and concise mental health notes using customizable templates. You can also invite clients to access their records through a secure and convenient patient portal and help them manage their health. To experience ICANotes and see how it works, sign up for your free trial or contact us today for more information.
Related Posts
Upcoming 21st Century Cures Act Changes
What You Need to Know About EHRs and Patient Privacy
Client Confidentiality: Best Practices for Behavioral Therapy Patients
Top 5 Reasons Behavioral Health Professionals Get Sued
Sources:
- https://www.opennotes.org/onc-federal-rule/
- https://www.psychologytoday.com/us/blog/digital-mental-health/202010/opening-mental-health-notes-7-tips-prepare-clinicians
- https://www.law.cornell.edu/uscode/text/42/1395u#b_18_C
- https://www.healthit.gov/cures/sites/default/files/cures/2020-08/Health_Care_Provider_Definitions_v3.pdf
- https://www.hhs.gov/hipaa/for-professionals/faq/2088/does-hipaa-provide-extra-protections-mental-health-information-compared-other-health.html
- https://www.hhs.gov/hipaa/for-professionals/faq/2094/does-parent-have-right-receive-copy-psychotherapy-notes-about-childs-mental-health-treatment.html
- https://www.healthit.gov/isa/united-states-core-data-interoperability-uscdi
- https://www.opennotes.org/about/
- https://www.opennotes.org/mental-health-professionals/
- https://jamanetwork.com/journals/jama/article-abstract/1853164
- https://www.opennotes.org/effects-of-opennotes-faqs/
- https://journalofethics.ama-assn.org/article/when-and-how-should-clinicians-share-details-health-record-patients-mental-illness/2017-03
- https://www.healthit.gov/cures/sites/default/files/cures/2020-03/InformationBlockingExceptions.pdf
- https://www.tandfonline.com/doi/abs/10.1080/09638237.2019.1644490
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5669408/
- https://depts.washington.edu/bhdept/ethics-medicine/bioethics-topics/articles/principles-bioethics
- https://www.opennotes.org/opennotes-for-health-professionals/
- https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2766834
- https://www.opennotes.org/ournotes-professionals/
- https://www.amjmed.com/article/S0002-9343(16)30548-4/pdf
- https://www.ccsa.ca/sites/default/files/2019-09/CCSA-Language-and-Stigma-in-Substance-Use-Addiction-Guide-2019-en.pdf
- https://www.apaservices.org/practice/update/2014/12-18/detailed-lean-records
- https://www.psychologytoday.com/us/blog/digital-mental-health/202004/should-psychotherapists-open-their-notes-patients