Mary Madison, RN, RAC-CT, CDP
Clinical Consultant – Briggs Healthcare
The Nursing Home Staffing Study Comprehensive Report – June 2023 was posted this afternoon.
This comprehensive report (478 pages) summarizes results from the Nursing Home Staffing Study activities between May and December of 2022 and presents options for minimum nurse staffing requirements for consideration by the Centers for Medicare & Medicaid Services.
From the Executive Summary…
In response to the White House call for action (February 2022), CMS contracted with Abt Associates to conduct a mixed methods Nursing Home Staffing Study as part of CMS’s multi-faceted approach to identify a minimum staffing requirement. The Staffing Study’s focus is on the level and type of staffing needed to promote acceptable quality and safety, so that residents are not at substantially increased risk of not receiving the safe and quality care they deserve. The study also explores potential implications for feasibility of increased staffing and costs to nursing homes. The Staffing Study was primarily conducted between May and December 2022, with some additional analytic work completed in 2023.
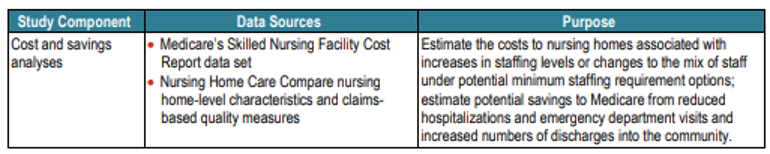
The goal of the Staffing Study is to identify a range of options to inform the development of CMS’s minimum staffing requirements, to promote quality and safe care for more than 1.1 million nursing home residents nationwide. The Nursing Home Staffing Study components illustrated in Exhibit ES.1 comprise a mixed-methods approach that characterized expected quality and safety outcomes as well as feasibility and costs across a range of minimum nurse staffing (registered nurse [RN], licensed practical/vocational nurse [LPN], and nurse aide) requirement options.

Below are key findings from the Staffing Study.
• Nurse staffing levels vary considerably across nursing homes nationwide, and by nursing home characteristics such as location, size, and profit status. Federal regulations require nurse staff availability 24 hours a day, but do not specify a minimum staffing level. Thirty-eight states and the District of Columbia have a minimum staffing requirement.
• Recent literature underscores the relationship between nursing home staffing and quality outcomes, such as reduced pressure ulcers, emergency department visits, rehospitalizations, and outbreaks and deaths related to COVID-19. However, it does not provide a clear evidence basis for setting a minimum staffing level.
• Nursing home staff, residents, and family members report that quality of life, quality of care, and resident safety are adversely affected when nursing homes are short staffed. Personal hygiene, especially bathing, and mealtimes are often affected. Short staffing also affects staff physical and mental health.
• Multivariate models show that quality and safety, as measured using claims, resident assessments, and health inspection data, increase with staffing levels, with no obvious plateau at which quality and safety are maximized or “cliff” below which quality and safety steeply decline.
• The relationship of staffing with quality and safety varies by staff type. Quality and safety consistently increase with RN staffing levels but only at the highest levels of nurse aide staffing. There is no consistent relationship of quality and safety with LPN staffing. There is a negative correlation between LPN and RN staffing, indicating that nursing homes with higher LPN staffing levels tend to have lower RN staffing levels.
• Multivariate models examined how the probability of exceeding quality and safety thresholds varied with nurse staffing levels, after accounting for differences in other nursing home characteristics. The Study Team established thresholds based on performance measures from the October 2022 Nursing Home Care Compare update. Quality thresholds were based on total quality measure performance (50th and 25th percentiles), and safety thresholds were based on within-state health inspection performance (50th and 25th percentiles). Based on observed associations from these models, the predicted percentage of nursing homes exceeding the current 25th (lowest quartile) or 50th (median) quality and safety performance percentiles would increase between 1 percentage point (~ 100 nursing homes) and nearly 8 percentage points (~1,200 nursing homes) across four potential minimum staffing requirement options ranging from low (below the current median) to high total nurse staffing.
• Simulation models indicate the percentage of clinical care either delayed or omitted decreases with greater licensed nurse (RN and LPN) staffing levels, falling below 10 percent at approximately 1.0 hour per resident day (HPRD) and approaching zero at approximately 1.4 HPRD. In combination with previous findings from the literature [13], this implies that a total nurse (RN, LPN, nurse aide) staffing level between 3.8 HPRD and 4.6 HPRD would be adequate to keep rates of both omitted activities of daily living care and omitted clinical care below 10 percent.
• A state-level minimum staffing requirement introduced in Massachusetts in 2020 penalizes its nursing homes with total nurse staffing below 3.58 HPRD with a 2 percent reduction in their quarterly Medicaid payments. This requirement increased staffing levels among low-staffed nursing homes with high Medicaid resident shares, with the effect most pronounced for nurse aides. However, the impacts of the requirement on quality and safety were not statistically significant. This may be related to findings in previous literature suggesting that modest increases in nurse aide staffing do not affect quality and safety. For safety outcomes, the lack of significant findings could also be related to data issues in health inspection measures. Specifically, as of December 2021, more than one-third of nursing homes did not have updated health inspection data since the beginning of the COVID-19 public health emergency (PHE) and the policy change.
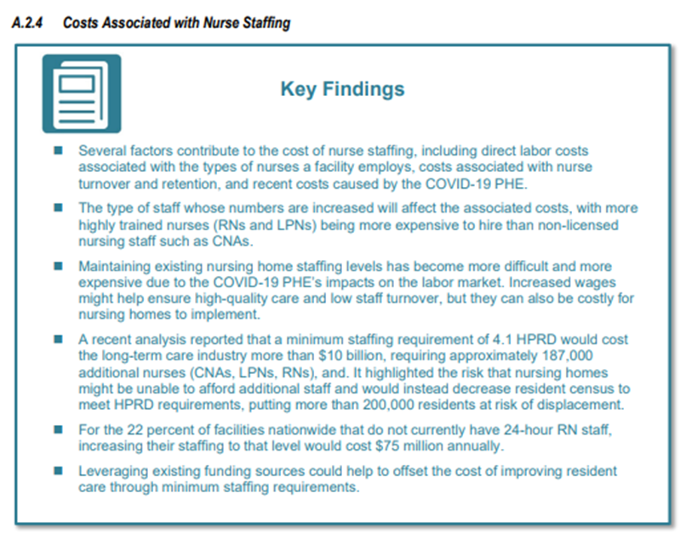
• The estimated minimum savings to the Medicare program specific to decreased use of acute care services and increased community discharges range from $187 to $465 million. There are many additional potential benefits that cannot be easily costed out because of data and time limitations, including those related to other clinical outcomes, out-of-pocket savings for residents, and improved resident quality of life.
• Nursing home staff and leadership report that nursing homes are currently very challenged in hiring and retaining direct care workers, because of workforce shortages and competition from higher-paying agency positions.
• Some stakeholders noted concerns about the lack of adequate current staffing to meet resident needs, while others raised workforce and cost considerations that could affect the feasibility of increased staffing. Many suggested considering resident acuity in setting a minimum requirement. Some stakeholders specifically highlighted the importance of staff training and skills.
• The total costs of additional staffing to meet a minimum staffing requirement range from $1.5 to $6.8 billion for the four potential minimum staffing requirement options presented in this report, and vary with the structure of the minimum requirement. Requirements structured to allow nursing homes flexibility to substitute across staff types to meet the requirement are generally less costly than requirements that do not allow for such substitution.
There is literally a plethora of information in the NH study. The Conclusion is found on pages 144 through 145 followed by the Glossary, References and Appendices.
Please share this study with your team and your colleagues. There’s a lot to talk about in this study!



Another news piece to digest along with this study is today’s KFF Health News Exclusive: CMS Study Sabotages Efforts to Bolster Nursing Home Staffing, Advocates Say by Jordan Rau.
“But a research study the Centers for Medicare & Medicaid Services commissioned to identify the appropriate level of staffing made no specific recommendations and analyzed only staffing levels lower than what the previous major federal evaluation had considered best, according to a copy of the study reviewed Monday by KFF Health News. Instead, the new study said there was no single staffing level that would guarantee quality care, although the report estimated that higher staffing levels would lead to fewer hospitalizations and emergency room visits, faster care, and fewer failures to provide care.
Patient advocates said the report was the latest sign that the administration would fall short of its pledge to establish robust staffing levels to protect the 1.2 million Americans in skilled nursing facilities. Already, the administration is six months behind its self-imposed deadline of February to propose new rules. Those proposals, which have not been released, have been under evaluation since May by the Office of Management and Budget. The study, dated June 2023, has not been formally released either, but a copy was posted on the CMS website. It was taken down shortly after KFF Health News published this article.
“It’s honestly heartbreaking,” said Richard Mollot, executive director of the Long Term Care Community Coalition, a nonprofit that advocates for nursing home patients in New York state. “I just don’t see how this doesn’t ultimately put more residents at risk of neglect and abuse. Putting the government’s imprimatur on a standard that is patently unsafe is going to make it much more difficult for surveyors to hold facilities accountable for the harm caused by understaffing nursing homes.””
The KFF News piece is also packed with information. At the end of the KFF News piece there is this update: [“This article was last revised at 3:30 p.m. ET to reflect that the Centers for Medicare & Medicaid Services removed a copy of the study from its website after this article was published, and to include reaction from CMS leadership and Abt Associates.”] I was able to pull down the Abt study from the website found in the 1st paragraph of this blog, which I authored an hour after finding the KFF News piece. If the hyperlink in the 1st paragraph doesn’t work for you, click on the hyperlink 3 paragraphs above, identified as the new study.
Both of these pieces are well-worth your attention. They are must-reads.

One thought on “Nursing Home Staffing Study Comprehensive Report Posted”
Comments are closed.