Mary Madison, RN, RAC-CT, CDP
Clinical Consultant – Briggs Healthcare

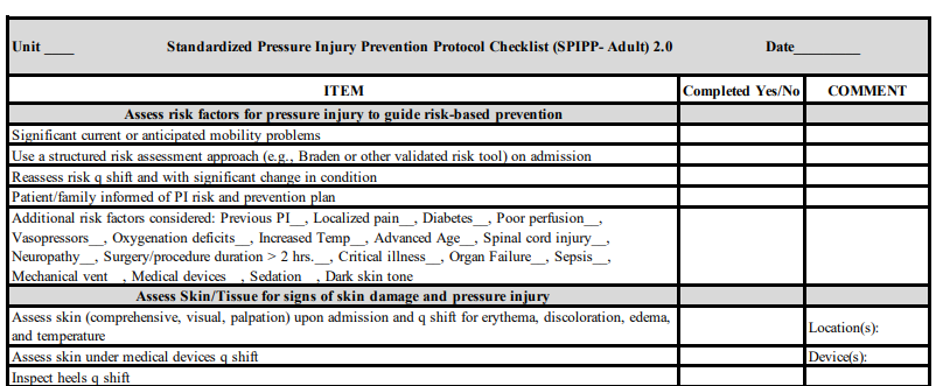
The National Pressure Injury Advisory Panel has released the second version of their Standardized Pressure Injury Prevention Protocol – abbreviated as “SPIPP” (pronounced S – PIP). The SPIPP is a shortened checklist of preventive actions to implement at the bedside, adapted from the 2019 Guidelines on pressure injury prevention. As the EPUAP-NPIAP-PPIA guideline has gotten longer, it was important to create a streamlined evidence-based operational approach to prevention.
The second version of SPIPP is directed at the critically ill patient. Immobility is the common denominator in the risk of pressure injury development. The first item in the SPIPP checklist addresses current or anticipated mobility problems as a risk factor. Consistent with the guideline, SPIPP states that clinical judgement should be used to refine risk assessment and SPIPP lists those risk factors to aid in identification of the additional risk. Methods to redistribute pressure for bedbound and chairbound patients are addressed – such as turning patients every 2-3 hours to a 30-degree lateral angle, and to use wedges and move the upper leg forward when the patient is on his/her side.
Patients with dark skin tones are addressed in SPIPP 2.0, noting darkly pigmented skin as a risk factor. There is guidance on how to inspect darker skin tones to determine areas of pressure injury when the skin remains intact. Enhanced assessment methods are also identified as a method to determine early signs of pressure injury.
Skin care actions in the SPIPP encourage managing moisture and incontinence with the use of urinary and fecal management systems for high-risk patients, keeping the skin clean and moisturized, and appropriately using low friction textiles/breathable pads/and wicking materials in skin folds. Nutritional interventions include a screening assessment for malnutrition on admission and when to notify the dietician – such as for patients with (or at risk for) malnutrition as well as when the patient is not eating, has been NPO for over 48 hours or has an open/ulcerated wound.
The document reminds the staff to explain to the patient and family the risk for pressure injury and the plan for prevention.
Using a panel of experts from across the United States, the SPIPP 2.0 demonstrated acceptable validity with a content validity index of 0.93. The SPIPP offers a realistic and practical method to ensure pressure injury prevention efforts are provided at the patient’s bedside.
The entire SPIPP 2.0 can be downloaded for free on NPIAP’s web site HERE.
If do not have an account with NPIAP, you must register to download this free 1-page document. You’ll register as a Guest.
Here’s a peek at that checklist:
If you’re familiar with the Braden Scale: Dr. Barbara Braden died in late June 2023. NPIAP honored the legacy of Dr. Braden with this posting on its website:
“NPIAP is saddened to share the news that Dr. Barbara Braden died last week. The National Pressure Injury Advisory Panel was honored to have Dr. Braden serve as a member of the Board of Directors. She is the 2019 recipient of the NPIAP JoAnn Maklebust Lifetime Achievement Award.

We knew her, of course, for her groundbreaking work in the development of a risk assessment tool to determine pressure sore risk. Its success was immediate and indisputable. A unique aspect of the tool is that all six areas of risk were areas that nurses could independently address. The tool does far more than evaluate risk! It provides a practical template for the risk-based prevention strategies needed to prevent pressure sores (injuries) in millions of at-risk patients. Dr. Braden’s pioneering tool – now known the world over as the Braden Scale – has become a key driver of quality care in hospitals and long-term care settings around the world. Validation of the Braden Scale was supported by a grant from the National Institute of Health (NIH). Dr. Braden’s seminal research, conducted in collaboration with Dr. Nancy Bergstrom, has served as a critical foundation for decades of subsequent pressure injury research.
Dr. Braden did much more for nurses and others in need. She was a Professor of Nursing at Creighton University and Dean of the Creighton University Graduate School. She developed and directed the Robert Wood Johnson Teaching-Nursing Home Project that nurtured a love for elder care in countless nursing students. She was an advocate for many groups served by Creighton University and the city of Omaha including the Nebraska AIDS Project and Nebraska Appleseed. She was passionately engaged with many national organizations. She had an enormous heart and wonderful, sharp sense of humor, along with an uncanny ability to tell a great story. NPIAP is thankful for her wisdom and wit, passion and perseverance, dignity and grace, and the immeasurable impact she has had on professional colleagues and the patients we serve. Barb, the gift of your life has enriched us all. Thank you!”
The Braden Scale was developed in 1988 and is still in use today. Indeed, thank you Dr. Braden for your service.
