This payer CEO topped Fortune's list of Most Powerful Women in Business
Fierce Healthcare
OCTOBER 5, 2021
This payer CEO topped Fortune's list of Most Powerful Women in Business. Tue, 10/05/2021 - 11:06.
This site uses cookies to improve your experience. By viewing our content, you are accepting the use of cookies. To help us insure we adhere to various privacy regulations, please select your country/region of residence. If you do not select a country we will assume you are from the United States. View our privacy policy and terms of use.

 payer-list
payer-list 
Fierce Healthcare
OCTOBER 5, 2021
This payer CEO topped Fortune's list of Most Powerful Women in Business. Tue, 10/05/2021 - 11:06.

Home Health Care
OCTOBER 5, 2023
Login The post What’s On Amedisys, VitalCaring, Intrepid’s Payer-Relationship Wish Lists appeared first on Home Health Care News. Right when I think I’ve written about the topic too much, I’m reminded again by a home health provider just how important it is. Sign up for HHCN+ to read this exclusive content.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.

Fierce Healthcare
SEPTEMBER 20, 2023
Veda, a data automation startup serving payers, has partnered with OutCare Health to help patients and payers identify queer-affirming providers. Data automation company Veda will ingest that information and offer it to payer clients. OutCare Health is known for its OutList, an extensive directory of LBGTQ+ affirming providers.

Fierce Healthcare
JUNE 7, 2023
Stemming the cost of cancer treatment tops the focus list of every payer. Cancer costs top the list of concerns for payers and employers alike. This oncologist and Chief Medical Officer offers savings strategies from PA do’s and don’ts to ways to address end-of-life costs.

Etactics
APRIL 26, 2024
On average, a healthcare provider has between 16 and 20 payer contracts. There’s no right answer, but understanding what a payer agreement is will show the significance of that average number. A payer commonly looks like insurance companies, government programs, and employers. There all different types of payers.
Healthcare ECONOMIST
FEBRUARY 14, 2024
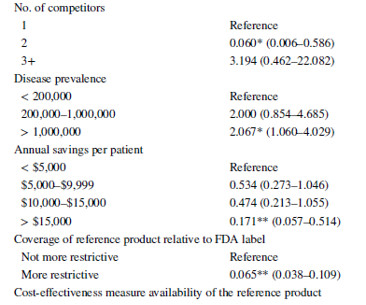
prior authorizations, step edits), we often think payers only use these for higher cost branded products including biologics. One question, however, is whether payers’ utilization management practices for biosimilars mirror those of biologic products, or small-molecule generics, or somewhere in between.
Etactics
APRIL 12, 2024
Table of Contents Third-Party Payers What’s a Clearinghouse? Just as insurance looks like a lot of different things, a third-party payer can look like a lot of different things. A third-party payer is any organization besides the patient that pays for healthcare services. Back to the basics. It’s a group effort. Not even close.
Healthcare ECONOMIST
MARCH 8, 2024
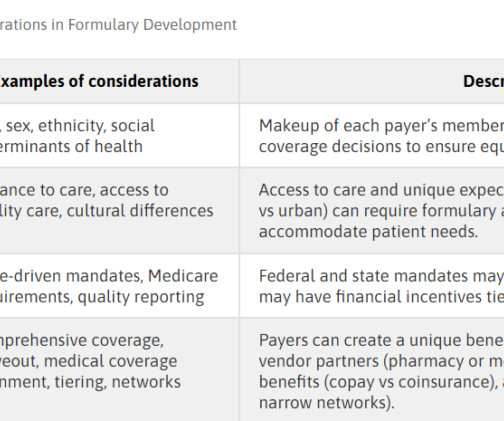
A formulary is a continually updated list of medications, products, and technologies supported by current evidence-based medicine, as well as the judgment of physicians, pharmacists, and other relevant experts in the diagnosis and treatment of disease and preservation of health. Below is a quick overview. What is a formulary?

HIT Consultant
MARCH 17, 2024
These new entrants are largely focused on offering primary care, urgent care, and a growing list of specialty services to make care more easily accessible, affordable, and cost-transparent. By working together with authentic data, both payers and retail health centers have a unique opportunity to significantly impact patient care.

HIT Consultant
APRIL 9, 2024
To address the benefit needs of underrepresented population groups, payers can develop “more equitable approaches to healthcare benefits design that recognize and meaningfully address access and affordability concerns,” according to a 2022 article in the American Journal of Health Promotion. And the list goes on.
Healthcare ECONOMIST
MARCH 26, 2024
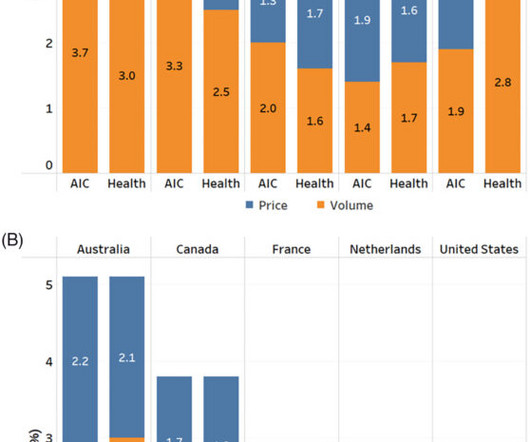
In the Figure below, spending growth is decomposed into prices and volume, where Panel A looks at consumption deflators for public payers and panel B looks at consumption deflators for private payers. out-of-pocket costs or private insurance). The full paper can be read here.

HIT Consultant
APRIL 26, 2024
This comprehensive care model empowers payers to better manage specialty drug costs. Wide Range of Medications: Access to a growing list of 240 limited distribution drugs, including exclusive options and medications in narrow networks. We have the flexibility to contract dynamically with any payer.

Healthcare It News
OCTOBER 4, 2022
CMS has provided payers with the option to implement a framework to show that they are connecting to HL7 FHIR APIs. Stakeholders who attain CARIN Code of Conduct Accreditation will be listed on the CARIN My Health Application site and the EHNAC Accredited Companies page.
Healthcare ECONOMIST
MARCH 11, 2024
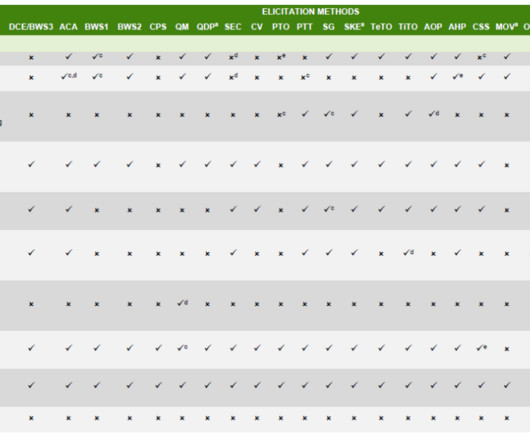
Payers make decisions for patients since–in most developed countries–third-party payment cover most of the cost. The PREFER methodology lists different types of methods from Soekhai et al. However, third parties often make decisions for patients. Physicians make decisions for patients due to asymmetric information (i.e.,

Healthcare It News
JULY 21, 2022
He said the deal represents an opportunity to help build a primary care experience with Amazon that's "more accessible, affordable, and even enjoyable for patients, providers, and payers." going forward.

Home Health Care
FEBRUARY 16, 2024
In general, the home health consulting firm SimiTree has noticed an increase in the amount of providers that have been struggling with things like unbilled claims, inaccurate primary payer selection and more, according to Lynn Labarta, vice president of post-acute revenue cycle management at SimiTree. We see this constantly.”

Healthcare It News
OCTOBER 13, 2022
Data tools are also high on the list of provider IT needs for FHIR adoption. The Centers for Medicare and Medicaid Services Office of the National Coordinator for Health Information Technology final rule prevents information blocking and promotes competition and innovation in healthcare IT.

Health Populi
FEBRUARY 13, 2024
Reviewing that list, starting with the great Dr. Tom Ferguson, one of Susannah’s mentors and many of our early role models working in what we then called eHealth, was a sweet d éjà vu. Here’s an initial list of Susannah’s Rebel Health book tour from the Penguin Random House site — keep checking it out for updates.

Home Health Care
JANUARY 3, 2024
The company plans to be listed on the Nasdaq, with the stock ticker BTSG. NYSE: JEF), Morgan Stanley (NYSE: MS) and Bank of America (NYSE: BAC), among others, acted as underwriters for the listing. KKR and an affiliate of Walgreens Boots Alliance (Nasdaq: WBA) acquired BrightSpring for $1.32 billion in 2019.

Sheppard Health Law
JANUARY 26, 2024
The payers impacted by the Final Rule include Medicare Advantage (“MA”) organizations, state Medicaid and Children’s Health Insurance Program (“CHIP”) agencies, Medicaid and CHIP managed care plans, and plans on the Affordable Care Act exchanges (collectively, “Impacted Payers”).

Home Health Care
JULY 20, 2023
As part of its business model, DocGo works with governments, health systems and payers. Under the partnership, HealthCare Partners NY will give DocGo a list of individual members that are non-compliant with these types of measures. Moving forward, DocGo plans to work with payers in a similar capacity.

p3care
SEPTEMBER 17, 2021
Medical billing software has been a blessing so far as it truly automates the way physicians interact with patients and payers (government or private). Here is a list of parameters that the RCM solution must be able to do. Such systems are fully automated to send notifications to patients and payers when required.

Etactics
MARCH 13, 2024
Fast forward to 100 years in the future, during the 1930’s the system evolved into the International List of Causes of Death. This allows payers to decide how a person will handle their payment responsibilities. For example, payers can determine which plan has the primary payment responsibility and how the other plans can contribute.
Briggs Healthcare
APRIL 4, 2022
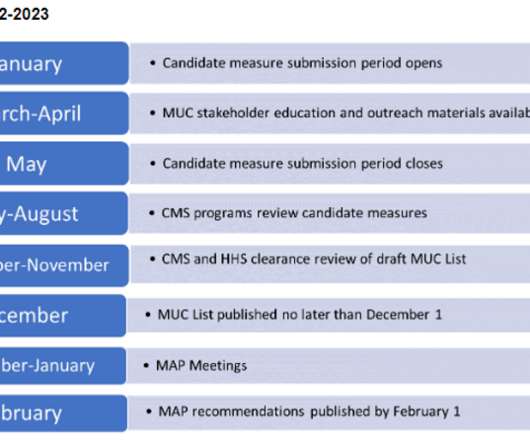
The pre-rulemaking process requires that HHS make publicly available, not later than December 1 annually, a list of quality and efficiency measures HHS is considering adopting, through the federal rulemaking process, for use in the Medicare program.

Healthcare ECONOMIST
MAY 11, 2023
You can list to the episode here (the segment on breast cancer screening starts at 5:32 ). Jason Shafrin on Marketplace Morning Report, May 11, 2023 I also weigh in on the provider impact as screening is often not well-reimbursed Costs are rising and reimbursement may be lagging especially for the public payers, Medicare and Medicaid.

Healthcare It News
MAY 5, 2022
So, real-time tracking of key indicators can help turn the corner, and communication between the provider, the patient and the payer team could make chronic care management work. Most are lab tests, but they are not assembled in a list for that specific disease. The payer part is an interesting sideline.

NASHP
APRIL 5, 2022
The tool also shows how those costs relate to both the hospital charges (list prices) and the actual prices paid by health plans. NASHP’s interactive Hospital Cost Tool provides anyone from policymakers to researchers with insights into how much hospitals spend on patient care services.
Health Populi
JULY 24, 2023
Here’s a list of the four categories of medicines on the GNC PRO “free formulary,” as it were. ” The quid pro quo value exchange is that GNC ramps up its membership list of consumers for the program and the promise of other purchases from the virtual or brick-and-mortar “front of the store.”

p3care
JUNE 21, 2023
To facilitate accurate billing and coding, the CMS offers a list of covered chiropractic codes. By doing so, chiropractic billing services can avoid claim denials and delays in reimbursement. Use of Chiropractic Modifiers Modifiers provide additional information about the chiropractic services rendered.

HIT Consultant
JULY 19, 2022
Jessica Bonham-Werling, Payer and Provider Solutions Marketing at Redox. America’s Health Insurance Plans (AHIP) recently assembled a truly impressive list of what health plans across the nation are doing. What my 3-year-old might call “a long, long, long, long time”. So in the meantime, what can be done?

Healthcare ECONOMIST
FEBRUARY 8, 2024
Understanding the economic impacts on patients and caregivers can help payers and other decision-makers to better design plans and strategies to ultimately improve patients’ experiences and outcomes. Economic Impacts. Scientific Spillover. IVI and AcademyHealth Economic Impacts Framework.

Etactics
NOVEMBER 3, 2022
Billing isn’t as simple as submitting a claim to a patient’s insurance payer, the payer reviewing the document, and you gett paid. Healthcare organizations use these documents for reimbursement from insurance companies (aka payers). These types of diagnoses come about as your treat the primary diagnosis listed in the header.

HIT Consultant
MARCH 16, 2023
Jim Collins, President of Medicare MSO Physicians need to keep their billing and coding right to ensure seamless reimbursements from payers. In addition, these codes help providers submit claims to payers and get paid for services. Similarly, there are additions in the list of telehealth services offered to patients.

Home Health Care
JANUARY 2, 2024
It’s one of the many payers that has prioritized home-based care as well. Devoted Health was also named to Fortune’s Best Workplaces in Health Care list and its Best Workplaces for Women list. Devoted, founded in 2017 by brothers Todd and Ed Park, was one of the first organizations to popularize the term “payvidor.”

Lexis Nexis
JULY 26, 2023
Enrollment fraud remains a major challenge for payers. So payers need a data analytics partner with the tools and expertise to stop bad actors in their tracks. They can help you set up early alerts and make dishonest enrollees stand out so it’s easier to root them out of your new member lists. It’s an unfortunate reality.

Home Health Care
MARCH 1, 2023
Referral sources] don’t want someone that just wants their fee-for-service [business] — they want to see a list,” she said. And then we get that to our payer innovation team, so that they can start further developing that pipeline.” They want to know that you really can be a more full-service provider.”

Home Health Care
SEPTEMBER 29, 2022
Two groups of stakeholders that home-based care providers need to win over in the near-term future are payer leaders and policymakers. In a world where the value of care is taking precedence over the volume of care, it’s important to show payers that home-based care is cost-effective and improves outcomes. “In Period” Korte said.

HIT Consultant
NOVEMBER 15, 2022
Payers, including insurance companies and government agencies, cannot help but look at the bottom line. Equipped with that knowledge, payers, pharma companies, and caregivers can better allocate their resources. Yes, the purpose of medical research is to save lives and improve the quality of life. But at what price?

Home Health Care
FEBRUARY 15, 2023
There are multiple hurdles to overcome for the company, which has been publicly listed for less than eight months. Those changes included the additions of a chief human resources officer and a “payer innovation team.” All the while, the payer innovation team is working hard at Enhabit to get more – and better – contracts with MA plans.

Icanotes
APRIL 13, 2021
It then reviews the claims before forwarding them to the payer, which is usually an insurance company. A payer can reject a claim if the codes aren't accurate, which can delay payment. Confirms compatibility: The clearinghouse verifies that the provider's claim is compatible with the payer's software, as well.

Sheppard Health Law
DECEMBER 15, 2022
The Proposed Rule, among other proposals, provides for new rules and standards for a payer-to-payer data exchange. In this post, we focus on the potential impact on MAOs of 1) the payer-to-payer data exchange and 2) prior authorization requirements. Payer-to-Payer Data Exchange Requirements.

Home Health Care
MAY 4, 2022
Aetna – one of the largest health insurance payers in the U.S. – That included the launching of “all-payer health products and services” to diversify the company’s growth portfolio and, more importantly, an “expansion of home health services.”. “But That] would make a lot of sense and they’d be high on the list.”.

Home Health Care
SEPTEMBER 21, 2023
This means diligence request lists, requests for information, management meetings, diligence calls and data rooms. Billing and coding claims reviews are conducted to make sure that the billing and coding that’s been done in the past is compliant with laws and payer requirements. “We The process becomes more formal.

Etactics
SEPTEMBER 28, 2022
An exact duplicate means that the payer determined that the same claim was already submitted in terms of… Date of service (DOS) Type of Service Provider number Procedure code of CPT Place of service (POS) Billed amount. Sometimes the payer has correctly identified that the claim is a duplicate of one already sent in. via Change.
Expert insights. Personalized for you.
We have resent the email to
Are you sure you want to cancel your subscriptions?

Let's personalize your content