CMS simplifying Medicaid, CHIP enrollment and renewal processes
Fierce Healthcare
MARCH 27, 2024
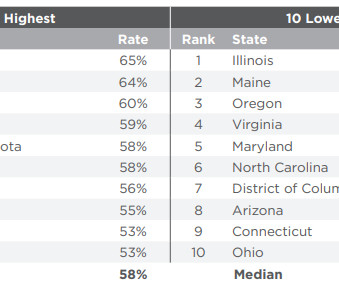
The Centers for Medicare & Medicaid Services (CMS) released a final rule Wednesday to help individuals obtain and retain Children's Health Insurance Program (CHIP) coverage. | In a final rule set to take effect in two months, CMS is streamlining its Medicaid and CHIP eligibility, enrollment and renewal processes.






































Let's personalize your content