What are Significant Requirements to become a QCDR in MIPS reporting?
p3care
JULY 16, 2023
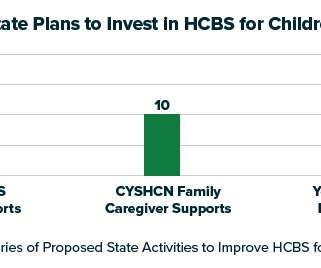
Mainly, these are the CMS-approved entities that collect and report clinical data from myriad resources. The resources can be electronic health records, patient surveys, and claims data. QCDR and QR are Not the Same Before moving to the main topic, please clarify one of the biggest confusions about QCDR. Now, let’s begin!























Let's personalize your content